Medical/Patient Care
Questions pertaining to medical or patient care
I have a potential patient with soft tissue radionecrosis secondary to colorectal cancer. He is currently undergoing chemotherapy with folfiri. Is there any contraindication to this drug in HBO?
Posted 6/23/25
Q:
I have a potential patient with soft tissue radionecrosis secondary to colorectal cancer. He is currently undergoing chemotherapy with folfiri. Is there any contraindication to this drug in HBO?
A:
“Folfiri is a very common chemotherapy drug cocktail for colorectal cancer and HBO2 is often used for radiation induced proctitis. There ar a handful of animal studies reporting 5Fu (the major component of Folfiri) using HBO2 as a sensitizer to increase the impact of 5FU with HBO2. To my knowledge none of these showed enhanced toxicities. The "Fol" part of Folfiri is folinic acid essentially a vitamin and no toxicity would be expected. The "iri" part is irinotecan. The mechanisms of Irinotecan are such that I would not expect increased side effects with HBO2.
See the following paper:
"Iyikesici MS. Long-Term Survival Outcomes of Metabolically Supported Chemotherapy with Gemcitabine-Based or FOLFIRINOX Regimen Combined with Ketogenic Diet, Hyperthermia, and Hyperbaric Oxygen Therapy in Metastatic Pancreatic Cancer. Complement Med Res. 2020;27(1):31-39. English. doi: 10.1159/000502135. Epub 2019 Sep 17. PMID: 31527373." this paper reports a human patient experience with Folfiri and several adjuvants, including HBO2. It did not report increased complications with this regime.
In this case, there is more info than typically available for a given chemo regimen and HBO2. With the above considerations, I believe that it is very unlikely that FOLFIRI and HBO2 will have increased toxicities. As always the decision to treat or not treat is the purview of the treating physician. I always recommend including the possibility of heightened side effects when we do not know the answer to this question with good evidence. My feeling is that there will not be increased complications. I would probably treat this patient as you you have described this patient.”
John Feldmeier, DO
I have a patient referral for HBOT and he is currently taking injectable Lupron Depot 22.5 mg QD a chemo drug for proste cancer. Is that compatiple with HBOT ?
Posted 5/6/25
Q:
I have a patient referral for HBOT and he is currently taking injectable Lupron Depot 22.5 mg QD a chemo drug for proste cancer. Is that compatiple with HBOT?
A:
Lupron is a blocker for testosrerone and I see no reason that it would interact negatively in any way with hyperbaric oxygen.
We have just gotten insurance authorization for a new HBOT order. When looking at her past medical history I see that she had a stapedectomy with an implant many years ago. The team requested an ID card but unfortunately this was placed 30 years ago so she has very minimal information of the details with this procedure. I would like to have your input for this. Have you dealt with or seen many hearing related implanted devices? How does that affect the patients HBOT?
Posted: 1/27/25
Q:
We have just gotten insurance authorization for a new HBOT order. When looking at her past medical history I see that she had a stapedectomy with an implant many years ago. The team requested an ID card but unfortunately this was placed 30 years ago so she has very minimal information of the details with this procedure. I would like to have your input for this. Have you dealt with or seen many hearing related implanted devices? How does that affect the patients HBOT? This is all the information available. NO name of the device
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
A stapedectomy is a procedure where the stapes bone is replaced by a prosthetic implant. Based upon experience of the physicians on our Safety Committee, a history of stapedectomy is a relative contraindication, and it may be possible to offer HBOT to this patient. Since the implant was placed some years ago, it should be stable and functional. The Committee recommends an ENT consultation and documented clearance before proceeding. If the original ENT who placed the implant is not available, we would recommend referral to an ENT specialist with interest or experience with SCUBA and/or hyperbaric oxygen therapy. The references below may add support for your decision.
Other Resources:
Diving after stapedectomy: Clinical experience and recommendations - ScienceDirect
Respectfully,
UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Hello. We have a potential patient who also receives regular molecular hydrogen inhalation therapy. Is there any contraindication to receiving HBOT concurrently? Should patient refrain from this other therapy during the course of HBOT?
Posted: 12/19/24
Q: We have a potential patient who also receives regular molecular hydrogen inhalation therapy. Is there any contraindication to receiving HBOT concurrently? Should patient refrain from this other therapy during the course of HBOT?
A:
As you might imagine, there is no real body of literature addressing this question. Hydrogen inhalation has become a very topical subject. No definitive clinical studies are available but pre-clinical research suggests that it may act as a reducer of inflammation and free radical damage.
In my search, I did find an article from 2023 that reports a fairly sizeable experience in applying hydrogen inhalation and hyperbaric oxygen for COVID patients. See article, click here.
For your patient, information related to the patient's chief complaint, pertinent history, and medications would be helpful in making a recommendation. The length of the planned treatment and specific hyperbaric protocol planned would also be helpful. What is the intent of the treatment.
The major take-home message for me from this attached article is that no increased toxicity was reported for this propensity-matched study when HBO and non-HBO patients were compared. All patients were receiving the hydrogen inhalation.
As always, the decision to treat or not treat a patient with a given therapy is the purview of the patient's managiing physician. However, based on the enclosed article, it does not appear that the concurrent treatment with hydrogen inhalation and hyperbaric oxygen is unlikely to cause unanticipated complications or side effects.
John J. Feldmeier, D.O.
I have a patient with a penile inplant that is fluid filled not air filled. It has not been tested for hyperbaric use, what are your thoughts on hyperbaric treatments
Posted: 12/16/24
Q: I have a patient with a penile inplant that is fluid filled not air filled. It has not been tested for hyperbaric use, what are your thoughts on hyperbaric treatments
A: “No contraindication here, as these are typically fluid filled. We responded to a similar product in 2021.” Click here
Weve been asked to treat patient for compromised graft. Pt has a history of coil embolization of left internal carotid arterial aneurysm2004. Results from 72024 MRA suggests possible residual flow within the aneurysmal neck vs flowinfundibulum at the origin of the eft anterior choroidal artery. Is it safe to treat?
Posted 10/18/24
Q:
We've been asked to treat patient for compromised graft. Pt has a history of coil embolization of left internal carotid arterial aneurysm2004. Results from 72024 MRA suggests possible residual flow within the aneurysmal neck vs flowinfundibulum at the origin of the eft anterior choroidal artery. Is it safe to treat?
A:
“Your concern about the coil in regard to hyperbaric treatments is probably related to the concern that the known impact on blood pressure in the chamber is to increase it, and that this increase might further dislodge the coil.
The paper by Heyboer does show an increase of pressure with HBO2, but this pressure increase is quite modest (on the order of 10mmHg). I doubt very seriously that a coil placed 20 yrs ago would be moved by such an increase in pressure. Of course , it would be helpful to review any earlier MRA studies to see whether the position and function of the coil have been stable over recent years.
In a situation like this, it is always useful to make contact with the other specialists including the group that placed the coil.
I searched to see if there was a published experience and could find none. As always, an informed consent is important in the vent that an unexpected or low probability would occur.
See the Heyboer paper. Effect of hyperbaric oxygen therapy on blood pressure in patients undergoing treatment
John J. Feldmeier, D.O.
Can you offer any information on an HBO treatment protocol for livedoid vasculopathy. There are a few case studies out there ranging from 1.4 ATA to 2.5 ATA for 1 hour, six day per week and all with similar conclusions of total wound closer and complete resolution of pain with no recurrence of ulcers after 6 to 8 month follow up.
Posted: 8/2/24
Q: Can you offer any information on an HBO treatment protocol for livedoid vasculopathy. There are a few case studies out there ranging from 1.4 ATA to 2.5 ATA for 1 hour, six day per week and all with similar conclusions of total wound closer and complete resolution of pain with no recurrence of ulcers after 6 to 8 month follow up.
A:
Please note that at the present time, the treatment of Livedoid vasculitis and certain other hypoxic wounds are not recognized as approved indications at this time.
A literature search was accomplished in an effort to determine whether there was any published material to provide guidance for responding to this question. There were very few articles that addressed this issue. Those that were available were case reports or small case series. Just as the individual who posed this question, I found when the pressures for treatment were reported, they varied from 1.45 ATA to 2.8 ATA. The paper advocating 1.45 ATA comes from Costa Rico by Herrera-Sanchez et al (Medicina (Buenos Aires) 2022 82:613-6.) Many of the Mild Hyperbaric documents advocate these low pressures primarily based on the false premise that treatments at this pressure are inherently safer and equally effective as standard pressures advocated by mainstream hyperbaric oxygen advocates. The Indications Manual 15th Edition, edited by Dr. Enoch Huang, now clearly defines clinical hyperbaric oxygen treatment as treatment occurring between 2.0 to 3.0 ATA. The chapter in this book by Huang et al discusses the mechanisms of hyperbaric oxygen in the treatment of chronic hypoxic wounds. The importance of adequate oxygen delivery and its impact on several biochemical events required to achieve a closed wound, including angiogenesis in the wound, are summarized here.
Transcutaneous oxygen assessment can be of use when selecting a treatment pressure. In diabetic foot ulcers, in a series of over 1000 patients, Fife et al have shown that transcutaneous measurements exceeding 200 mmHg in the chamber during treatment are needed to predict an improved likelihood of healing (Fife CE, Smart DR, Sheffield PJ, Hopf HW, Hawkins G, Clarke D. Transcutaneous oximetry in clinical practice: consensus statements from an expert panel based on evidence. Undersea Hyperb Med. 2009 Jan-Feb;36(1):43-53. PMID: 19341127. These patients were treated at 2.0 and 2.4 ATA. Likewise, Sheffield and co-authors had reported that transcutaneous measurements done with a challenge of 100% oxygen accomplished at ground level demonstrated a better outcome when this level was greater than or equal to 150% of the value obtained on ground-level air when the raw value exceeded 35 mmHg (Hyperbaric Oxygen Treatment Of Hypoxic Wounds Sheffield PJ, Dietz D, Posey KI, Sheffield JC, *Bakken B. Nix Wound Healing Center, San Antonio, Texas 7820).
Admittedly, these publications were for diabetic foot ulcers, not livedoid vasculitis ulcers. However, I believe it is widely accepted that the successful treatment of livedoid ulcers requires the delivery of adequate oxygen pressures to carry out the numerous steps involved in healing hypoxic wounds, similarly to diabetic ulcers. It should be noted that most of the reviewed case reports and small series employed 2.5 ATA for their hyperbaric oxygen treatments.
Therefore, my preference and advice to the individual in selecting treatment pressures is to continue to employ pressures of 2.0 to 2.5 ATA for which there is over than 50 years of experience.
John JH. Feldmeier, D.O.
We have a patient with recent bilateral mastectomy and tissue expanders. What are the requirements if expanders are filled with air vs. saline for treating in hyperbaric? This question is urgent as the indication is flap failure.
Posted 7/11/24
Q: We have a patient with recent bilateral mastectomy and tissue expanders. What are the requirements if expanders are filled with air vs. saline for treating in hyperbaric? This question is urgent as the indication is flap failure.
A:
Patients referred for acute vascular ischemia of the breast tissue following mastectomy, including nipple areola complex ischemia, are referred for hyperbaric oxygen treatment (HBO2) in an attempt to arrest the ischemia and hypoxia produced from the extensive dissection necessary during the mastectomy.
First, tissue expanders used in breast reconstruction are almost always filled with saline. Here are some key points regarding the use of saline versus air:
- Saline: The standard practice is to fill tissue expanders with saline. Saline is preferred because it is not compressible under pressure changes, such as those experienced during hyperbaric oxygen therapy and air travel. This stability mitigates risk best with saline-filled expanders and more predictable as fluid does not respond to pressure changes in a hyperbaric chamber, pressurized aircraft, or moving from areas of high pressure to low pressure and vice versa.
- Air: Filling tissue expanders with air is extremely uncommon. Air-filled expanders are susceptible to compression and expansion with changes in atmospheric pressure posing risks in environments such as hyperbaric chambers, during flights in pressurized aircraft, and changes in atmospheric pressure from location to location. The use of air-filled expanders is typically limited to temporary situations or specific clinical scenarios where immediate, short-term expansion is needed, and the patient is not exposed to significant pressure changes.
Clinical Practice: Tissue expanders are usually filled with saline to mitigate risk and better ensure patient safety and optimal outcomes in various clinical situations and environmental pressure change.
To safely proceed with hyperbaric oxygen treatment and prevent worsening ischemia, it is recommended that:
- Tissue expander volume should be reduced: Remove enough saline (or air) from the expanders to decrease stress and tension on tissue and suture lines. This reduces pressure on the breast tissue, which could be contributing to the ischemia.
- If volume reduction is not possible: Remove the expanders as soon as feasible to alleviate pressure on the surrounding vessels post-mastectomy.
This approach ensures the patient can undergo HBO2 while minimizing the risk of exacerbating the ischemia.
In cases where tissue expanders are inserted following a bilateral mastectomy, where significant tissue removal has occurred, the immediate post-operative filling of tissue expanders requires careful consideration on the part of the plastic surgeon:
- Immediate Post Operative Filling: Typically, tissue expanders are filled with a small amount of saline at the time of placement to maintain their position and avoid collapse. This initial fill should be minimal to reduce the risk of excessive pressure on the newly operated tissue.
- Gradual Expansion: The expansion process should be gradual and carefully monitored. Regular follow-ups with the surgeon are necessary to incrementally increase the fill volume, allowing the tissue to stretch slowly and reducing the risk of complications such as ischemia or undue pressure on the tissue.
- Consideration of Ischemia Risk: In patients at risk of ischemia, particularly those referred for hyperbaric oxygen treatment, it may be prudent to delay significant filling of the expanders until the risk of ischemia has been thoroughly assessed and managed.
- Customizing to Patient Needs: The decision should be individualized based on the patient's condition, the extent of tissue removal, and the surgeon’s judgment. Close monitoring for signs of ischemia or other complications is essential.
In summary, while tissue expanders can be initially filled post-operatively, the volume should be minimal, with careful and gradual expansion thereafter. The specific approach should be tailored to the patient's needs and clinical situation, particularly if there is a significant risk of ischemia or ischemia becomes apparent. This response addresses the concerns about using HBO2 treatment with tissue expanders and provides guidelines for managing such cases.
Owen ONeill, MD, MPH, FUHM, FACHM
Taxotere and HBO2: Are there known complications or contraindications?
Posted; 7/23/24
Q:
Taxotere and HBO2: Are there known complications or contraindications?
A:
Literature Search: A literature search was accomplished by me. No specific publications were found that reported unexpected or unexpectedly severe complications of Taxotere when given concurrently with hyperbaric oxygen.
Introduction: Taxotere is a member of the class of chemotherapy drugs called Taxanes, which also includes Taxol. It works to inhibit cancer cell mitosis by interfering with the tubules that participate in that part of mitotic reproduction.
The Tables below give the common and the severe complications caused by this drug.
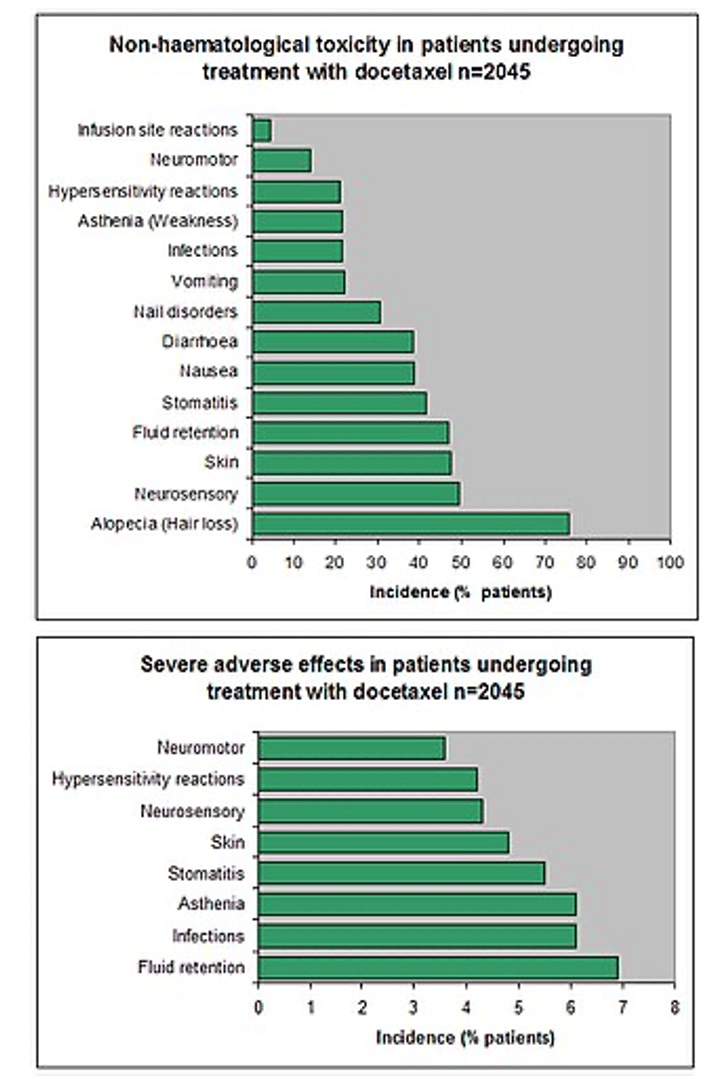
Note, these tables were taken from the Wikipedia write up of Taxotere.
Of note, GI effects are common, and when patients are treated in the chamber, diarrhea may occur and be difficult to manage in that environment.
Also, fluid retention is reported as a potentially severe complication which could increase the likelihood of CHF and flash pulmonary edema which as you know can occur in the chamber. Patients should be checked daily for fluid retention and respiratory deterioration.
Finally , a lung complication abbreviated DPLD (diffuse parenchymal lung disease) can be a fatal pulmonary complication of Taxotere. Patients should be carefully monitored for this complication.
There are no specific complications that would be expected to be exacerbated specifically due to high doses of oxygen given while the patient is being treated with Taxotere.
Since there is no published experience for the interaction of the 2 modalities, knowledge of the kinetics of the drug can be helpful. Three different serum half lives are reported for the drug. The longest of these is 12.2 hours. It is commonly administered by IV infusion every 3 weeks. After the passage of 5 half lives (5 X 12.2 hours) or 61 hours ( just a little over 2 days), the concentration of the drug will have fallen to about 3% of the maximum dose. I would recommend that a short interruption of the HBO2 occur to allow clearance of the drug to that level. If Taxotere is given on a Friday, by Monday, the levels will be below 3%. By reducing the drug concentration to such a low level, the potential for interactions of the riuch oxygen environment and the drug should be minimized.
As always, the decision to treat a patient with HBO2 is the purview of the physician who will be in charge of the treatment and has seen the patient in person and given an informed consent.
John J. Feldmeier, D.O.
Does a patients A1C need to be below a certain number before HBO tx is beneficial?
Posted: 6/20/24
Q: Does a patients A1C need to be below a certain number before HBO tx is beneficial?
A:
No. The question is if the email is referencing the wound care literature, which is split between those who feel better control equates to better outcomes and those who believe that all patients deserve a trial.
If the question is referencing the requirement for DFU and HBOT, then the question is more about documenting an A1C and then referring them to a nutritionist/PCP for counseling and intervention. There is a schism even within the diabetes community as to what constitutes good control; it varies depending upon the age of the patient and the co-morbidities.
https://diabetesjournals.org/care/article/46/Supplement_1/S216/148044/13-Older-Adults-Standards-of-Care-in-Diabetes-2023
Whether or not they have significant autonomic dysfunction and can sense hypoglycemia is a major risk factor that needs to be addressed.
There are multiple examples in the literature where A1C and outcomes are not linked in the hyperbaric medicine space.
Helen Gelly, MD, FUHM, FACCWS, UHM/ABPM
Thank you.
What is the main concern or danger with a systolic blood pressure below 100 pre HBO treatment assessment?
Posted:11/13/23
Q:
What is the main concern or danger with a systolic blood pressure below 100 pre HBO treatment assessment?
A:
There is nothing magic about a systolic BP less than 100mmHg in the hyperbaric environment. Various authors have studied the impact of BP as the result of hyperbaric treatments. We know that HBO2 causes arteriolar constrictions and increased afterload, sometimes leading to the occurrence or worsening of CHF. For most patients, the changes are negligible. But for a patient with hypotension in the chamber, the tendency is for a BP increase not a decrease.
I am not sure where you got this guidance. I would like to know for future reference. The thinking, I believe, arises out of caution because 100 mmHg systolic is a fairly low pressure and may be due to sepsis or blood loss. More than anything, I believe whoever authored this policy was trying to alert the treating HBO2 doctor that the patient may be having significant intercurrent disease symptoms and should be stabilized before going into the chamber.
There is a subset of slight young women who characteristically will run blood pressures like this. It is therefore important to get the patient’s history or check previous medical trecords to determine if this is a normal and usual pressure for your patient.
John J. Feldmeier, D.O.
Any contraindication treating patient with patent foramen ovale?
Posted: 5/25/23
Q: Any contraindication treating patient with patent foramen ovale?
A: In the general population 30% of individuals have a PFO. Individuals with a PFO have a slightly increased risk of decompression sickness (DCS). However, the risk of DCS for a patient undergoing hyperbaric oxygen treatment is zero. Thus, for patients undergoing HBO2 treatment the presence of a PFO is irrelevant.
Radiation cystitis withOUT hematuria: One of our urologists would like to refer patients with incapacitating symptoms of radiation cystitis (frequency, urgency, etc) and evidence of "necrosis" on cystoscopy but no gross hematuria. He has anecdotal evidence that these symptoms improve with HBOT. Is there any support from the literature and /or would cystitis withOUT hematuria be covered by Medicare?
Posted: 5/19/23
Q: Radiation cystitis withOUT hematuria: One of our urologists would like to refer patients with incapacitating symptoms of radiation cystitis (frequency, urgency, etc) and evidence of "necrosis" on cystoscopy but no gross hematuria. He has anecdotal evidence that these symptoms improve with HBOT. Is there any support from the literature and /or would cystitis withOUT hematuria be covered by Medicare?
A: From Dr. Helen Gelly, “CMS covers both codes N30.40 and N30.41.” Please see linked excel spreadsheet for reference.
- Excel spreadsheet: Click Here
Just wondering if the ejection fraction guidelines have changed, we have always followed the greater than 30%, or 25 to 30% if stable, would get cardiac clearance if needed, and what would be considered unstable? clearance if needed, and what would be considered unstable?with cardiac clearance if their
Posted: 10/11/2022
Q:
Just wondering if the ejection fraction guidelines have changed, we have always followed the greater than 30%, or 25 to 30% if stable, would get cardiac clearance if needed, and what would be considered unstable? clearance if needed, and what would be considered unstable?
A:
Re: Left ventricular ejection fraction and hyperbaric oxygen:
This answer originates from Dr. Neil Hampson, M.D who is the retired long term medical director of the Virginia Mason Hyperbaric unit. Dr. Hampson is board certified in Internal Medicine, Pulmonary Medicine, Critical Care and Hyperbaric Medicine. Of course, in addition to the left ventricular ejection fraction, the patient’s recent cardiac history should be obtained and considered. If the patient has recently required medical intervention for cardiac failure issues especially if frequently recurrent, this factor should be included into the decision making in regard to the treatment with hyperbaric oxygen for a non-emergent condition. It is always prudent to consult the patient’s cardiologist when there are concerns about the possibility of inducing congestive heart failure with hyperbaric oxygen treatments.
Here are Dr. Hampson’s recommendations:
Cardiac Screening for HBO2:
- History of cardiac disease – ask to see patient’s last CXR and review last echocardiogram report
- If echocardiogram is greater than one year old and was abnormal, repeat it
- If last echo of any age showed LVEF > 40%, repeat only if cardiac symptoms have progressed since that time
- If echocardiogram performed within one year shows:
- LVEF >30% Proceed with HBO2
- LVEF 20-30% Involve cardiology for optimization prior to considering HBO2
- LVEF <20% No routine HBO2
Is hereditary spherocytosis a contraindication to hyperbaric oxygen treatments?
Posted 6/7/22
Q:
Is hereditary spherocytosis a contraindication to hyperbaric oxygen treatments?
A:
Sporadically, there is mention in literature that hyperbaric oxygen may cause increased hemolysis for patients with hereditary spherocytosis. In my search, I was unable to find an original reference citing an organized study or even a case series or case report demonstrating increased hemolysis for spheroid cytosis patients treated with hyperbaric oxygen. I suspect (but cannot prove) that some where along the line, some one speculated that since hyperbaric oxygen causes vasoconstriction that abnormally shaped red blood cells and prone to hemolysis would have more mechanical stress and therefore more hemolysis. Although spherocytosis is relatively rare, I suspect that patients with spheroid cytosis have been previously treated perhaps inadvertently, and we have no reports of increased hemolysis.
I recommend that you include in your informed consent a statement to the effect that some have suggested that there may be increased hemolysis for spheroid cytosis patients undergoing hyperbaric oxygen but that there are reports of patients treated without toxicity. A weekly CBC during treatment would also be prudent, and if there are signs of increased hemolysis, HBO2 should be discontinued and the patient should see his or her hematologist.
should HBOT treatment be added to debridement and IV antibiotics for soft tissue clostridium infection
Posted: 5/20/22
Q:
Should HBO2 treatment be added to debridement and IV antibiotics for soft tissue clostridium infection?
A:
Hyperbaric oxygen has been a mainstay in the treatment of Clostridial necrotizing soft tissue infections since the pioneering work of Brummelkamp in Holland in the 1960’s. This work was done along with much of the early work that established hyperbaric oxygen as an appropriate adjunctive treatment for several disorders that we continue to treat. The initial rationale was Clostridial organisms are anerobic bacteria and would likely find hyperbaric oxygen lethal or at least bacteriostatic.
Liquefactive soft tissue necrotizing infections can be caused by several Clostridial species including C. perfringens (the most common) along with C. oedematiens, C. septicum, C. histolyticum, C. bifermentans, and C. fallax. More recent investigation of the Clostridial species causing gas gangrene have shown that they are not strict anerobes. Clostridial perfringens will grow freely in oxygen tensions as high as 30mmHg with some growth even up to tissue oxygen tensions of 70mmHg.
The clostridial organisms release at least 20 toxins which are largely responsible for the lethality and toxicity of the disease. The most studied and most important of these is called alpha toxin. This toxin is responsible in large part for the rapidly spreading liquefactive necrosis which is a prominent feature of the serious infections we know as gas gangrene with the local necrotizing process advancing more than one inch every hour. This toxin also plays a large part in causing systemic toxicities.
Four distinct levels of severity have been described. These include: 1) Diffuse clostridial necrosis with systemic toxicity (true gas gangrene); 2) Localized Clostridial myonecrosis; 3) Clostridial cellulitis with systemic toxicity; and Clostridial cellulitis without toxicity.
Clinical signs of gas gangrene include a mild fever (100 to 101 degrees), a tachycardia of 150 beats per minute or higher which is disproportionately elevated for the fever, and a peculiar sort of sensorium where the patient is intellectually aware of the seriousness of their infection but is emotionally unconcerned, also called “la belle indifference.” Interstitial gas is often shown on radiographic studies. Clinically crepitus may be palpated.
Hyperbaric oxygen should be part of a combined modality therapy including high dose antibiotics and surgical debridement. Hyperbaric oxygen is very useful in helping to distinguish between permanently destroyed damage versus salvageable tissues. We recommend against amputation immediately unless the limb is absolutely and certainly beyond salvage and instead recommend hyperbaric oxygen be initiated prior to any radical surgeries. The intent here is to identify and save as much viable tissue as possible. Antibiotics typically include penicillin and/or clindamycin.
Early diagnosis is generally made by history along with a gram stain of the wound which will show large gram positive rods.
The spectrum of effects of Clostridial infections includes respiratory, cardiac, renal complications and DIC. Often these patients will require heparin therapy.
The most important effect of hyperbaric oxygen appears to be the shut down of further alpha toxin production if/when tissue oxygen tensions are increased to 250 mmHg or higher. Oxygen tensions of 2000 or more mmHg are cytotoxic but may not be achieved in vivo.
Patients with trauma or pre-existing vasculopathies including diabetes are at higher risk for gas gangrene. A common source for gas gangrene is a contaminated wound in a patient with impaired circulation. Gas gangrene can occur post operatively, but compared to trauma this occurrence is relatively rare.
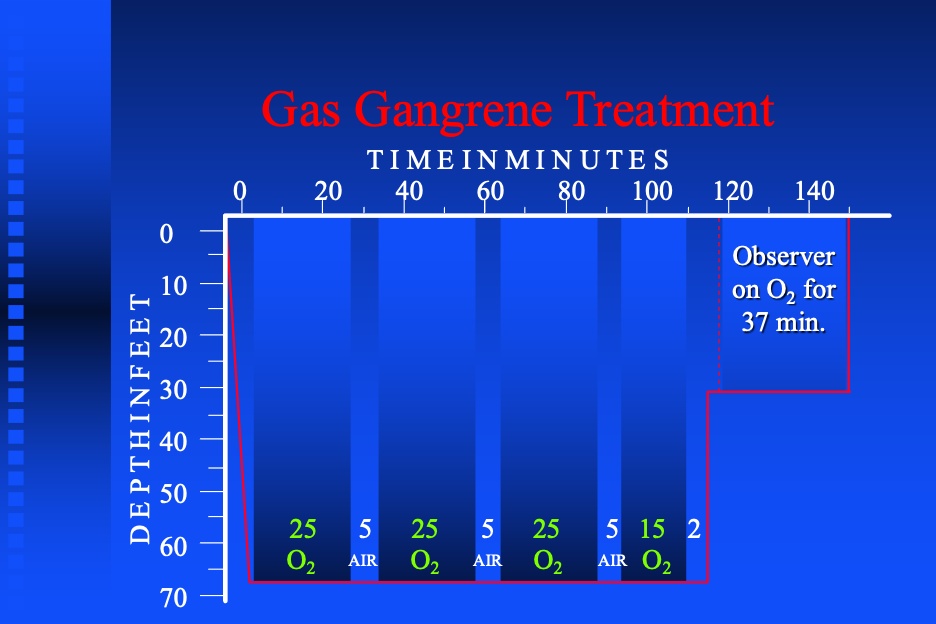
In order to have the best impact of hyperbaric oxygen on the infection as part of the multi-disciplinary management, it is necessary to treat these patient at high pressures and multiple times daily typically for 3 days. Typically 3 treatments are given in the first 24 hours and then BID treatments for the next 2 days. In this writer’s experience, oxygen induced seizures are fairly common because these patients are toxic and treated at high pressures of 3.0 ATA. This usually requires a modification in treatment profile to allow continuation of treatment. Since it is important to achieve high treatment pressures and high tissue oxygen levels in the tissues, it is preferrable to shorten oxygen periods over reducing treatment pressure.
All standard textbooks of hyperbaric oxygen deal present extensive information on the treatment of gas gangrene. The treatment of gas gangrene is one of the 14 indications approved by the UHMS. The Indications Manual 14th Edition is a good reference as well as the Whelan-Kindwall textbook or the Neuman-Thom textbook.
Note: see a typical treatment profile below:
A woman called to ask whether we treated post covid-19 symptoms. She has had many issues including severe fatigue, brain fog, difficulty sleeping and states that she is desperate. She is apparently part of a support group; several people have evidently benefitted from HBOT. Does anyone have any experience treating these folks? The patient is willing to pay out of pocket, but I wonder if there are any institutions with ongoing research studies. We are a small monoplace operation without any capability of d
Posted: 2/14/22
Q:
A woman called to ask whether we treated post covid-19 symptoms. She has had many issues including severe fatigue, brain fog, difficulty sleeping and states that she is desperate. She is apparently part of a support group; several people have evidently benefitted from HBOT. Does anyone have any experience treating these folks? The patient is willing to pay out of pocket, but I wonder if there are any institutions with ongoing research studies. We are a small monoplace operation without any capability of doing controlled studies. Any thoughts would be appreciated. Thank you.
A:
There is no central registry of hyperbaric centers that are treating patients for the persistent symptoms of COVID-19 (the so called “Long Haulers”). Through the “Grapevine” we have heard that several centers are treating these patients. The treatment pressures have varied from less than 2.0 ATA to 2.8 ATA and treatment times of 60 to 90 minutes. Typically, the number of treatments has ranged from 5 to 20 in number.
There are 2 clinical trials registered on the NIH site, clinicaltrials.gov, that are conducting studies of HBO2 for Long Haulers. One from Israel with Dr. Efrati as lead investigator and listed on this website as completed, but no results are available yet. A second study by the Karolinska Institute from Stockholm, Sweden is listed as ongoing. The lead investigator is not given on the website. No co-investigating researchers or institutions in the U.S. are mentioned on the website. On an earlier study, Dr. Pieter Lindholm at the University of California, San Diego had been listed as a co-investigator, and he may have additional information. Otherwise, we would advise that the patient in question make contact with hyperbaric facilities near her home to determine if any are doing such treatments for this patient group. Since many hyperbaric centers have popped up recently that are not treating approved indications and have inadequate medical supervision and resulting safety concerns, we recommend that she determine whether the centers she contacts are treating only approved indications or on clinical trials. A good indicator for the quality of a center’s practice is to determine whether they are treating only approved indications or patients on studies with an occasional treatment outside this guidance for compassionate purposes. We recommend she inquire as to whether the center and its staff are members of the UHMS (Undersea and Hyperbaric Medical Society) or at least follow the recommendations of the UHMS. This recommendation is made because the Society has established high standards for the practice of Hyperbaric Medicine which can be dangerous if not properly delivered. Another good indicator of the quality and safety of the delivery of hyperbaric oxygen is to ensure that a licensed physician is always present during the treatment.
The Society cannot make a broad recommendation advocating hyperbaric oxygen for COVID long haul patients. We recognize that there are physiologic effects of Hyperbaric Oxygen which may be helpful in the treatment of COVID-19. Also, we are aware of unpublished reports that hyperbaric oxygen seems to have been successful in the treatment of some symptoms that persist after the acute infection. We do encourage participation in clinical trials whenever possible. We anxiously await the results of the pending clinical trials. We also recognize that the treating physician is ultimately the decision maker when it comes down to recommending and offering hyperbaric oxygen for a given health problem. As always, he or she needs to consider the potential benefits versus the possible side effects or complications of the therapy.
I have a 62 y/o patient with radiation cystitis who has already received a total of 80 HBO treatments over the course of 10 months (March 2020-December 2020) for recurrent hematuria. He recently had another episode of hematuria that was treated with clot irrigation only (no cautery needed). He was referred back to me by his urologist. Is there any utility to additional treatment with HBO, given that he has already had 80 treatments within the last 2 years? I realize this is technically a new episode o
Posted: 2/8/2022
Q:
Would it be likely effective to offer more HBO2 to an 62 y/o patient who has already completed 80 HBO2 treatments over 10 months (March-December 2020) for recurrent hematuria?
A:
A few additional bits of information would be helpful. Apparently, the patient had a cessation of hematuria for a at least a short time in December 2020. When did the patient have recurrence of hematuria? What type of tumor did the patient have? Do you have any information on radiation dose or technique-specifically was there an implant or was IMRT the treatment technique? Has the patient required transfusion? Is the patient getting chemotherapy for residual or recurrent tumor?
I share your concerns that it is probably unlikely that additional hyperbaric treatments at this point will be effective. However, I have personal experience with radiation cystitis patients who had durable response after up to 100 treatments. I have also seen patients respond to a second course of treatment after a resolution followed by recurrence.
I would recommend that the patient have a cystoscopy at this time. If the site of hematuria is focal, a local intervention with chemical or electrocautery should be considered. If it is diffuse, the instillation of formalin should be considered. If these are not appropriate or possible and the patient is willing, though unusual, additional Hyperbaric oxygen is a reasonable option. As always, especially, if the tumor was a bladder cancer to begin with, recurrent cancer should be ruled out.
I have a 40 y/o patient with a large open lower leg wound (lower thigh/popliteal fossa) with an underlying diagnosis of mycoses fungoides. He has had radiation therapy on three separate occasions since 2016 with total dose of 7000cGy, however each treatment episode was not more than 3000cgy. Recent wound biopsies still show tumor. His family is pushing for HBO to try to heal the wound, as his oncology team is reluctant to consider stem cell transplant until the wound is healed. I have 2 questions: 1)
Posted: 2/8/2022
Q:
I have a 40 y/o patient with a large open lower leg wound (lower thigh/popliteal fossa) with an underlying diagnosis of mycoses fungoides. He has had radiation therapy on three separate occasions since 2016 with total dose of 7000cGy, however each treatment episode was not more than 3000cgy. Recent wound biopsies still show tumor. His family is pushing for HBO to try to heal the wound, as his oncology team is reluctant to consider stem cell transplant until the wound is healed. I have 2 questions: 1) his only current treatment for the tumor is Bexarotene (he has failed treatment with multiple other chemotherapy agents) and I can\'t find much info on this. Is it safe in conjunction with HBO? Does it affect wound healing? 2) In terms of possible contribution of prior radiation to poor healing, can I consider this is a possibility even though the total radiation dose was delivered in multiple treatment episodes over more than 5 years?
A:
Background:
Mycosis fungoides (MF) is a primary lymphoma of the skin due to T-Cell lymphocytes. MF is responsible for about 40% of primary skin lymphomas. As an aside T-Cell lymphocytes are responsible for cellular immune response. They directly kill the infecting organism; whereas, B-cell lymphocytes produce antibodies, and it is these antibodies that are the primary effect of B-Cell response and control of infecting organisms. Mycosis fungoides typically presents as a plaque-like, often confluent, sometimes nodular, often erythematous dermatitis. It is often very pruritic. I will attach a photo. It is not typically ulcerative though some of the lesions may demonstrate focal ulcerations. Often times the diagnosis is delayed for years (5-8 years). Survival after diagnosis is 5 to 8 years. Organ involvement is unusual early on but is present in 80% of those who die of their disease.
Oncologic treatment is often dictated by the extent of the disease. If it is localized a local radiation field is often used. If it is generalized, chemotherapies often one of the new targeted or immunologic agents are used. If lymph nodes are involved the prognosis is worse. If there is involvement of internal organs, prognosis is worse yet again. Very early mycosis is often treated with topicals including steroids and some chemo agents. Sometimes a technique of whole-body electron treatment is done for diffuse skin involvement. Ultraviolet light has been used with response in early cases in a technique termed PUVA which uses type A ultraviolet light. More recently systemic agents are used for diffuse involvement. These agents are not typically traditional cytotoxic chemotherapy but are targeted or immune therapies. Drugs used include the monoclonal antibodies Brentuximab and Mogamulizumab. Interferon has also been used for treatment as a modulator of immune response. By the way, Bexatrone is a retinoic acid (Vitamin A). it induces cell differentiation and apoptosis and prevents the development of drug resistance. Note: It also has anti-angiogenic effects and inhibits cancer metastasis. There is some experience with high dose chemotherapy and stem cell transplant but this experience is somewhat limited. Really. In almost all cases curative treatment is not possible but the course of the disease is typically long and theoretically at least it can be prolonged with intervention.
Image of Mycosis Fungoides (pdf)
Your Case:
In general, skin lesions that have tumor in them will not heal. This experience has been seen in primary skin cancers (basal and squamous cells) and lymph nodes with metastatic disease that ulcerate through the skin.
You note that the patient has had 3 prior courses of radiation with a total dose of 7000 cGy and wonder about the time interval between treatment courses and whether late radiation effects are likely to occur. Some in the radiation community believe that the radiated tissues will with time between treatment courses recover radiation tolerance. In my experience, that is certainly not always true and the late effects of the separate courses are additive. Also often, MF patients are treated with treatment fractional doses at 300 or even 500 cGy. These higher than the normal daily dose of 180 to 200 cGy are in fact more damaging for a given total dose. Therefore, I believe that this could well in part be late radiation damage.
I believe offering the patient hyperbaric oxygen is a reasonable option. A trial of therapy for perhaps 20 daily treatments is advised. If the patient is not showing expected response at that point, I believe that the presence of tumor in the lesion is the culprit. Of course the reason that transplant is being held is that the conditioning high dose chemotherapy would be very immunosuppressive and put the patient at risk for cellulitis perhaps advancing to sepsis. It is also possible that the anti-angiogenic effects of Bexatrone will work against the HBO2.
By the way, please let us know how the patient does. It will increase our knowledge. A positive outcome would make a good case presentation because of the rarity of the clinical challenges you face.
I have a patient referred to me for treatment of soft tissue radionecrosis of oral mucosa of rt posterior maxilla and posterior rt mandible. Patient has undergone radiation and chemotherapy for carcinoma rt tonsillar fossa and tongue. He is cancer free but has ulceration in treated areas. Oncology has biopsied these areas and no recurrences. Do I have to wait 6 months from therapy to start treatment?
Posted: 7/12/2021
Q:
I have a patient referred to me for treatment of soft tissue radionecrosis of oral mucosa of rt posterior maxilla and posterior rt mandible. Patient has undergone radiation and chemotherapy for carcinoma rt tonsillar fossa and tongue. He is cancer free but has ulceration in treated areas. Oncology has biopsied these areas and no recurrences. Do I have to wait 6 months from therapy to start treatment?
A:
You do not mention how long ago the radiation and chemotherapy were completed or how extensive or deep the ulcerations are.
Also if these ulcerations are at the site of the tumor, it may take a period of time for the body to replace this site with normal tissues after the cancer has been eradicated.
If this is indeed radiation necrosis of the soft tissue, I know of no constraints or prohibition in initiating hyperbaric oxygen. Generally, these types of lesions are painful and interfere with eating. Hyperbaric oxygen should hasten their resolution. You may want to contact the insurance carrier ahead of time and explain the case to guarantee appropriate reimbursement.
EARLY HYPERBARIC OXYGEN THERAPY FOR REDUCING RADIOTHERAPY SIDE EFFECTS: EARLY RESULTS OF A RANDOMIZED TRIAL IN OROPHARYNGEAL AND
NASOPHARYNGEAL CANCER;
Int. J. Radiation Oncology Biol. Phys., Vol. 75, No. 3, pp. 711–716, 200
I recently saw a 52-year-old male with a hx of anaplastic oligodendroglioma, referred by his neuro-oncologist for possible hyperbaric oxygen therapy treatments for brain radiation necrosis and worsening cognitive impairments. In April 2019, the patient had a left craniotomy for removal of a large frontal tumor with hemorrhage and herniation with pathology of anaplastic oligodendroglioma WHO grade 3. He had radiation therapy (5940 cGy) July-August 2019 and concurrent TMZ (Temozolomide) chemotherapy. A
Posted: 5/17/2021
Q:
I recently saw a 52-year-old male with a hx of anaplastic oligodendroglioma, referred by his neuro-oncologist for possible hyperbaric oxygen therapy treatments for brain radiation necrosis and worsening cognitive impairments. In April 2019, the patient had a left craniotomy for removal of a large frontal tumor with hemorrhage and herniation with pathology of anaplastic oligodendroglioma WHO grade 3. He had radiation therapy (5940 cGy) July-August 2019 and concurrent TMZ (Temozolomide) chemotherapy. After a stereotactic brain biopsy of lesion in left splenium of the corpus callosum in November 2020, he was placed on Bevacizumab for radiation necrosis.
Patient had a stereotactic left-brain biopsy in early May 2021 for a worsening corpus callosum lesion. Pathology report: necrotic brain parenchyma with rare intermixed atypical cells, suspicious for tumor.
The next day, the pathology report shows “ …. This confirms that he does have a recurrence of oligodendroglioma, as the cause of the enlarging lesion. There is also a significant element of necrosis present, with diffuse (not nodular/necrotic) tumor.”
Patient is on a nine-day dexamethasone taper to see if it will help improve his cognition, and the patient is about to start chemotherapy: PCV (procarbazine/CCNU/vincristine) with a port being placed for the vincristine.
I am reluctant to treat the radiation necrosis while he is undergoing active cancer therapy.
I would like to get your thoughts about this situation.
A:
These cases are always difficult because there are so many chemo agents now including targeted therapies. biologics and immune enhancing agent.
If the patient has had Bevacizumab in the past 4 months, I would not treat him with HBO. The drug is an angiogenesis inhibitor, specifically VEGF. As we know HBO works at least in part by inducing angiogenesis as one of the major growth factors. Intuitively, applying both simultaneously would have you working against yourself. Supposedly, it gives some palliation of brain necrosis by stabilizing vascular integrity and preventing or at least ameliorating interstitial edema.
The new drugs are all well-known and have been around for a while. Procarbazine is an alkylating agent. It works to inhibit DNA, RNA and protein synthesis. CCNU is also known as Lomustine. It is also an alkylator. It is known to lipid soluble and for this reason has better penetration into the brain than many other chemo agents. Vincrisine is in a class of drugs called vinca alkaloids. It inhibits microtubule formation within the cell to prevent successful mitosis. Since this patient has likely combination of tumor necrosis and persistent tumor, it makes your decision even more difficult. One of the characteristics of high-grade brain tumors is necrosis. It is possible to my reading that his problems are all due to tumor. I predict his symptoms will get worse as they taper the decadron.
With HBO2 effects on reducing edema, you may get some near immediate improvement in his brain function. With a persistent or recurrent high-grade tumor his survival is probably measured in less than 6 months. From my investigations, I have found no evidence that you will cause the tumor to be more aggressive. It is going to be aggressive whether you give him HBO2 or not. In terms of the chemo complications being worse with concurrent HBO2, it is impossible to say. Alkylators are said to be radiomimetic. In other words, they cause breaks in DNA strands mediated through free radicals. You may actually provide some sensitization of the tumor to the chemotherapy in the same fashion O2 sensitizes tumors to radiation damage.
I would wait until they have completed their taper of steroids in any case. I expect they will have to return him to the steroids. As sad as it is there is little we can do for this patient and it may be time to pull the plug on therapies.
We currently have a patient with RTI to head and neck. She had HBO in 2011 and 2012 for ORN of the mandible. She is now having an extraction of a tooth and surgeon is ordering 10 HBO post extraction. We follow the protocol of 20/10 HBO as stated in our LCD in Penna.from 2019. Many years ago we followed a protocol of 10 HBO post extraction if patient had HBO within 5 years of new extraction. This patient is 9 years post HBO. What is the protocol that we should be using? We do not have a new LCD to follow.
Posted: 2/22/2021
Q:
We currently have a patient with RTI to head and neck. She had HBO in 2011 and 2012 for ORN of the mandible. She is now having an extraction of a tooth and surgeon is ordering 10 HBO post extraction. We follow the protocol of 20/10 HBO as stated in our LCD in Penna.from 2019. Many years ago we followed a protocol of 10 HBO post extraction if patient had HBO within 5 years of new extraction. This patient is 9 years post HBO. What is the protocol that we should be using? We do not have a new LCD to follow.
A:
Dr. Marx who designed the protocols believes, based on transcutaneous measurements he has done on a group of patients 2 and even 3 yrs. out from HBO2, that improvement in the radiation damaged vascularity is permanent. He saw no regression in levels obtained immediately after completion of the HBO2 when compared to the 2 and 3 yr. measurements post HBO2. He does not recommend pre-extraction HBO2 for patients who have had 2 prior courses or even 1 prior course of HBO2 with either the 20/10 in association with extractions or a 30/10 course for the treatment of existent ORN. The 10 post-extraction HBO2 treatments are prudent in my judgement. If the patient were to have delayed healing with exposed bone after these ten, consideration to perhaps an additional 10 to 20 treatments could also be considered. If healing after the 10 post-extraction is progressing nicely, no additional treatments will be needed. If the oral surgeon finds more ORN at the time of the extractions, consideration should be given to a full forty treatments to treat recurrent ORN
We currently have a patient with RTI to head and neck. She had HBO in 2011 and 2012 for ORN of the mandible. She is now having an extraction of a tooth and surgeon is ordering 10 HBO post extraction. We follow the protocol of 20/10 HBO as stated in our LCD in Penna.from 2019. Many years ago we followed a protocol of 10 HBO post extraction if patient had HBO within 5 years of new extraction. This patient is 9 years post HBO. What is the protocol that we should be using? We do not have a new LCD to follow.
Posted: 2/19/2021
Q:
We currently have a patient with RTI to head and neck. She had HBO in 2011 and 2012 for ORN of the mandible. She is now having an extraction of a tooth and surgeon is ordering 10 HBO post extraction. We follow the protocol of 20/10 HBO as stated in our LCD in Penna.from 2019. Many years ago we followed a protocol of 10 HBO post extraction if patient had HBO within 5 years of new extraction. This patient is 9 years post HBO. What is the protocol that we should be using? We do not have a new LCD to follow. The doctor is questioning the 20 treatments pre extraction.
A:
Dr. Marx who designed the protocols believes, based on transcutaneous measurements he has done on a group of patients 2 and even 3 yrs out from HBO2, that improvement in the radiation damaged vascularity is permanent. He saw no regression in levels obtained immediately after completion of the HBO2 when compared to the 2 and 3 yr. measurements.. He does not recommend pre-extraction HBO for a patient like yours who has had 2 prior course of HBO2. The 10 post-extraction HBO2 treatments are prudent in my judgement. If the patient were to have delayed healing with exposed bone after these ten, consideration to perhaps an additional 10 to 20 treatments could also be considered. If healing after the 10 post-extraction is progressing nicely, no additional treatments will be needed.
I have a 45 y.o. M with hx of R sudden hearing loss and hx of posterior fossa approach for brain tumor removal, and still has a right posterior ventriculoperitoneal catheter. He needs hyperbaric tx for sudden hearing loss of now L ear. Is it safe to dive a patient with VP cathether
Posted: 3/2/2021
Q:
I have a 45 y.o. M with hx of R sudden hearing loss and hx of posterior fossa approach for brain tumor removal, and still has a right posterior ventriculoperitoneal catheter. He needs hyperbaric tx for sudden hearing loss of now L ear. Is it safe to dive a patient with VP catheter?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
For the sake of the reader who may not be familiar with this device, a ventriculoperitoneal catheter (or shunt) is used to drain excess cerebrospinal fluid (CSF) from the brain. The shunt works by moving fluid out of the brain by way of a one-way valve with reservoir connected to a short and long catheter routed to the abdomen where the fluid can be absorbed. This lowers the pressure and swelling on the brain.
The UHMS HBO2 Safety Committee observes that this device is fluid-filled and should behave similarly compared with other fluid lines and drains that are consistently allowed in chambers. One concern may be the lack of access and fluid control that the provider may have to the patient if therapy is provided in a monoplace chamber. We recommend that these and all other risks to the patient are identified in a risk assessment performed by the Safety Director and Medical Director of your facility. We also recommend reaching out to the device manufacturer, as there are programmable versions of these shunts with greater complexity.
There is at least one published article describing a successful test of a VP shunt under Hyperbaric conditions, “Ventriculo-peritoneal shunt performance under hyperbaric conditions.” The Safety Committee reached out to one of the authors of this article, who stated: “This testing was performed on a specific Medtronic VP shunt. Theoretically if the shunt is all fluid filled and had no mechanical parts, it should function as intended under hyperbaric conditions. We did the testing just to confirm that it did, but I would recommend that whomever is treating the patient should go through the same thought process (not necessarily the testing) as they would to evaluate any equipment that is to go in the chamber.”
Other considerations and observations from the UHMS HBO2 Safety Committee include:
- I have treated a few patients with these over the years. I have approached their approval-to-dive as I would for any other fluid filled and fully implanted device.
- Think of the VP shunt like a siphon. It is fluid filled, so generally there no worries with HBOT unless this shunt is in an inside attendant. There is an underlying reason (usually hydrocephalus) that would make me think twice about subjecting an employee to pressure routinely.
- There might be an extra consideration depending on how the back-check valve operates for a given device, but I’ve only seen ones that open based on elevated ICP and not any biomechanical process that universally applied pressure or oxygen gradients would affect. Still always double check with the manufacturer every time, though.
- We have treated numerous patients with a VP shunt and as the shunt is fluid filled it has not been an issue.
- We have routinely allowed patients with the older non-programmable shunts to go into the chamber. We also let the newer programmable devices in. However, the last time we checked they were not formally pressure tested by the manufacturer. The manufacturer did have reports of their shunts in the HBO environment without issue. I haven’t contacted the company of late.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
Burman, F. (2019). “Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities,” (6th ed.). San Antonio, TX: International ATMO, Inc.
Huang ET, Hardy KR, Stubbs JM, Lowe RA, Thom SR. “Ventriculo-peritoneal shunt performance under hyperbaric conditions.” Undersea Hyperb Med. 2000 Winter; 27(4):191-4. https://pubmed.ncbi.nlm.nih.gov/11419359/
Memorial Sloan Kettering Cancer Center, “About Your Ventriculoperitoneal (VP) Shunt Surgery.” Accessed 02/26/2021. https://www.mskcc.org/cancer-care/patient-education/about-your-ventriculoperitoneal-vp-shunt-surgery
DISCLAIMER
Is there any reason/ caution to take in diving an 80 y/o woman s/p resection of left jaw and tongue for SCC 1982- post radiation. During her resection the vagus phrenic nerve was cut resulting in paralysis of her left diaphragm. I spoke with her pulmonologist. He states she has 47% lung capacity, mild asthma and OSA. He states he knows nothing about HBO and cannot say whether she would be safe diving or not. She runs an 88-94% O2 on room air. She is not on supplemental O2 and is asymptomatic- no SOB. The
Posted: 2/12/2021
Q:
Is there any reason/ caution to take in diving an 80 y/o woman s/p resection of left jaw and tongue for SCC 1982- post radiation. During her resection the vagus phrenic nerve was cut resulting in paralysis of her left diaphragm. I spoke with her pulmonologist. He states she has 47% lung capacity, mild asthma and OSA. He states he knows nothing about HBO and cannot say whether she would be safe diving or not. She runs an 88-94% O2 on room air. She is not on supplemental O2 and is asymptomatic- no SOB. The plan is to dive her for orn with dental caries and dry mouth- in need of dental extraction with pre/post HBOT @ 2.5ATA w/ 2 air breaks x 20 up front and 10 after tx.
A:
From a safety point of view, assuming she doesn’t have bullous disease she should be fine with HBO2 unless she is a CO2 retainer (baseline hypercapnia). If her PCO2 is significantly elevated (i.e. greater than 48 mmHg) she may become more hypercapnic in the chamber, which would predispose her to CNS O2 toxicity.
However, with her baseline hypoxemia it is possible she may not achieve a therapeutic PO2 during hyperbaric therapy. If her asthma is under good control I suggest obtaining a baseline ABG on room air, from which her PO2 during HBO2 could be estimated.
I completed an HBO consult on a patient regarding a wound in an irradiated area. He is currently on cabozantinib regarding metastatic renal cancer. My question is, the mechanism of action of this chemo medication in inhibiting VGEF resulting in decrease angiogenesis. Is this reason not to treat him? Won’t this be going against the benefit of HBO trying to promote angiogenesis? Thank you for any input.
Posted: 2/3/2021
Q:
I completed an HBO consult on a patient regarding a wound in an irradiated area. He is currently on cabozantinib regarding metastatic renal cancer. My question is, the mechanism of action of this chemo medication in inhibiting VGEF resulting in decrease angiogenesis. Is this reason not to treat him? Won’t this be going against the benefit of HBO trying to promote angiogenesis? Thank you for any input.
A:
Cabozantinib and HBO2:
As the writer has pointed out, this drug interferes with VEGFR2 (One of 3 receptors for vascular endothelial growth factor). This receptor is involved in wound healing.
I also agree that using it with hyperbaric oxygen is likely to diminish the effectiveness of HBO2 in promoting angiogenesis as an essential part of wound healing.
Another potential effect is by providing more VEGF activity, the HBO2 may diminish the effectiveness of the drug in its impact on the cancer.
We do not have any published clinical experience with the combination of the 2 modalities. However, based on an understanding of their mechanisms and common sense, I would recommend not giving HBO2 and Cabozantinib concurrently.
It has a fairly long serum half life (120 hours) and has been shown to increase fivefold in concentration over a fifteen day administration.
See abstract below:
Clinical Pharmacokinetics and Pharmacodynamics of Cabozantinib
Steven A Lacy 1, Dale R Miles 2 3, Linh T Nguyen 2 4
Affiliations expand
- PMID: 27734291
Abstract
Cabozantinib inhibits receptor tyrosine kinases involved in tumor angiogenesis and metastasis. The capsule formulation (Cometriq®) is approved for the treatment of progressive metastatic medullary thyroid cancer at a 140-mg free base equivalent dose. The tablet formulation (Cabometyx™, 60-mg free base equivalent dose) is approved for the treatment of renal cell carcinoma following anti-angiogenic therapy. Cabozantinib displays a long terminal plasma half-life (~120 h) and accumulates ~fivefold by day 15 following daily dosing based on area under the plasma concentration-time curve (AUC). Four identified inactive metabolites constitute >65 % of total cabozantinib-related AUC following a single 140-mg free base equivalent dose. Cabozantinib AUC was increased by 63-81 % or 7-30 % in subjects with mild/moderate hepatic or renal impairment, respectively; by 34-38 % with concomitant cytochrome P450 3A4 inhibitor ketoconazole; and by 57 % following a high-fat meal. Cabozantinib AUC was decreased by 76-77 % with concomitant cytochrome P450 3A4 inducer rifampin, and was unaffected following administration of proton pump inhibitor esomeprazole. Cabozantinib is a potent in vitro inhibitor of P-glycoprotein, and multidrug and toxin extrusion transporter 1 and 2-K, and is a substrate for multidrug resistance protein 2. No clinically significant covariates affecting cabozantinib pharmacokinetics were identified in a population pharmacokinetic analysis. Patients with medullary thyroid cancer with low model-predicted apparent clearance were more likely to dose hold/reduce cabozantinib early, and had a lower average dose through day 85. However, longitudinal tumor modeling suggests that cabozantinib dose reductions from 140 to 60 mg/day did not markedly reduce tumor growth inhibition in medullary thyroid cancer patients.
Under UHMS and/or CMS guidelines, can HBO therapy be utilized to support artificial skin grafts? If so, are there any ways which approach to use of HBOT might differ from support of a compromised flap/graft?
Posted: 1/12/2021
Q:
Under UHMS and/or CMS guidelines, can HBO therapy be utilized to support artificial skin grafts? If so, are there any ways which approach to use of HBOT might differ from support of a compromised flap/graft?
A:
These are the ICDs for compromised graft that are approved for treatment with HBO2. By definition, autograft and allograft can’t be artificial.
996.52 Mechanical complication due to graft of other tissue, not elsewhere classified T86.820 Skin graft (allograft) rejection
996.52 Mechanical complication due to graft of other tissue, not elsewhere classified T86.821 Skin graft (allograft) (autograft) failure
996.52 Mechanical complication due to graft of other tissue, not elsewhere classified T86.822 Skin graft (allograft) (autograft) infection
996.52 Mechanical complication due to graft of other tissue, not elsewhere classified T86.828 Other complications of skin graft (allograft) (autograft)
Is it acceptable to have a Certified Medical Assistant performing hyperbaric treatments? I have heard of it in the past but wasn't sure if it is still acceptable. I do know that they cannot certify anymore unless they have a current EMT status.
Posted: 12/15/2020
Q:
Is it acceptable to have a Certified Medical Assistant performing hyperbaric treatments? I have heard of it in the past but wasn\'t sure if it is still acceptable. I do know that they cannot certify anymore unless they have a current EMT status.
A:
Thank you for your question!
I’ve included the link to the UHMS’s PS on certification - https://www.uhms.org/images/Position-Statements/position_statement_-_uhms_associates_hyperbaric_certification_recognition_v.10.05.2019_v6_1.pdf.
A CMA does qualify as a qualifying pathway for the ABWH’s CWS exam and certification but not for the NBDHMT’s CHT. Those links are listed below.
https://abwh.net/get-certified/certified-hyperbaric-specialist/
https://www.nbdhmt.org/forms/CHT_Resource_Manual.pdf - qualifying pathway page 1
What is the best approach of treating pediatric patients in monoplace chambers? Is it safe to allow a parent inside the chamber with the child?
12/21/2020
Q:
What is the best approach of treating pediatric patients in monoplace chambers? Is it safe to allow a parent inside the chamber with the child?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee is aware of several facilities that allow this practice, provided that several risk mitigations are in place prior to therapy. While NFPA-99 classifies chambers based on occupancy, Class A (human - multiple occupancy) or Class B (human - single occupancy), the document does not prohibit this practice. The Food and Drug Administration allows the Off-Label Use of Medical Devices under the Supervision of a Physician and subject to certain, safety-based criteria. We suggest applying this principle to the scenario above.
The UHMS HBO2 Safety Committee recommends that the Hyperbaric Medical Director and Hyperbaric Safety Director examine the risks and benefits of this approach with each particular patient and consider the safety mitigations described below before proceeding with this practice. We also recommend that the facility develop standardized procedural guidance for this scenario ahead of time and discuss the approach with the hyperbaric staff. There may be the need to gather information from your legal and administrative teams before engaging in this practice, so we encourage that procedural guidance and equipment needs are ready before the consult is realized.
Please consider the following safety mitigations and recommendations pertaining to the practice of the treatment of a patient with an occupant caregiver in the monoplace chamber:
- We recommend that the occupant caregiver be a parent, guardian or relative that is well known to the patient. If possible, try to maintain consistency with that individual throughout the treatment plan.
- Have a plan in the event that the primary occupant caregiver is unable to be in the chamber, so as not to interrupt the treatment plan for the patient.
- We recommend grounding both the patient and the occupant caregiver, and test the continuity of both devices prior to every therapy.
- An individual breathing apparatus should be available for each occupant where air breaks are used.
- Consider the use of “wye” connections for grounding and air break purposes.
- Ensure that the air break mask is properly suited for the adult/pediatric patient, as applicable.
- The Hyperbaric Physician should provide thorough education to the occupant caregiver and provide instruction on how to respond to the side effects of therapy
- The Hyperbaric Physician should evaluate the occupant caregiver for the risks of hyperbaric oxygen therapy and gain consent as they would a patient.
- The facility should have a plan to respond to an incapacitated occupant caregiver (seizure activity, cardiac arrest, etc.).
- Consider documenting in the occupant caregiver’s chart and treating this as a separate appointment
- Consider a nominal or ‘no-charge’ visit for the occupant caregiver
- Avoid the use of clinical staff as occupant caregivers – the oxygen exposure creates an additional occupational risk and may be a complicated matter from the perspective of occupational health and human resources (job description/job expectations). Consult with these groups before considering this approach.
- Anticipate the need to consult with your hospital’s Administration, Safety Management, and Legal teams. Ensure that any safety, liability, or reimbursement concerns are addressed.
Also noteworthy, the National Board of Diving and Hyperbaric Medical Technology released a statement in 2011 related to this practice:
“…the Board of Directors has posted a new Position Statement (July 2011; 2011-02). It relates to the not uncommon practice of having a pediatric patient accompanied in a monoplace chamber. The decision to require a staff or family member to join such patients is entirely that of the treating hyperbaric physician and presumably a decision based upon a risk-benefit assessment. It is not the intent of this latest Position Statement to argue the relative merits of this practice. Rather, the Board wants to ensure that should dual occupancy occur it does so with relevant safety standards considered.” Link
References:
Optimizing the pediatric hyperbaric oxygen therapy plan: Tandem therapy - Nicholas Marosek, RN, CHRN, UHMS Safety Pre-Course, June 2019
Celebi, A. R. C., Kadayifcilar, S., & Eldem, B. (2015). Hyperbaric oxygen therapy in branch retinal artery occlusion in a 15-year-old boy with methylenetetrahydrofolate reductase mutation. Case reports in ophthalmological medicine, 2015.
Fok, T. F., Shing, M. K., So, L. Y., & Leung, R. K. W. (1990). Vascular Air Embolism‐Possible Survival. Acta Pædiatrica, 79(8‐9), 856-859.
Hsieh, W. S., Yang, P. H., Chao, H. C., & Lai, J. Y. (1999). Neonatal necrotizing fasciitis: a report of three cases and review of the literature. Pediatrics, 103(4), e53-e53.
Korambayil, P. M., Ambookan, P. V., Abraham, S. V., & Ambalakat, A. (2015). A multidisciplinary approach with hyperbaric oxygen therapy improve outcome in snake bite injuries. Toxicology International, 22(1), 104. Liebelt, E. L. (1999).
Hyperbaric oxygen therapy in childhood carbon monoxide poisoning. Current opinion in pediatrics, 11(3), 259-264.
Mader, J. T., Adams, K. R., Wallace, W. R., & Calhoun, J. H. (1990). Hyperbaric oxygen as adjunctive therapy for osteomyelitis. Infectious disease clinics of North America, 4(3), 433-440.
Smith-Slatas, C. L., Bourque, M., & Salazar, J. C. (2006). Clostridium septicum infections in children: a case report and review of the literature. Pediatrics, 117(4), e796-e805.
Tsung, J. W., Chou, K. J., Martinez, C., Tyrrell, J., & Touger, M. (2005). An adolescent scuba diver with 2 episodes of diving-related injuries requiring hyperbaric oxygen recompression therapy: a case report with medical considerations for child and adolescent scuba divers. Pediatric emergency care, 21(10), 681-686.
Waisman, D., Shupak, A., Weisz, G., & Melamed, Y. (1998). Hyperbaric oxygen therapy in the pediatric patient: the experience of the Israel Naval Medical Institute. Pediatrics, 102(5), e53-e53.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We treated a patient recently with hemorrhagic cystitis secondary to BK virus.(40 treatments, 6/11/20-8/11/20) He has a history of CML. In the last 2-3 weeks the patient has had a recurrence of hematuria "dependent on hydration" and the team has reached out to us for more treatments. Do you think more treatments would be efficacious?
Posted: 10/16/2020
Q:
We treated a patient recently with hemorrhagic cystitis secondary to BK virus.(40 treatments, 6/11/20-8/11/20) He has a history of CML. In the last 2-3 weeks the patient has had a recurrence of hematuria "dependent on hydration" and the team has reached out to us for more treatments. Do you think more treatments would be efficacious?
A:
I did a search and have seen Dr. Moon's reply. As he said there may be a role for hyperbaric oxygen in hemorrhagic cystitis in leukemic patients who have stem cell transplants for their leukemia. In my reading up to 50% of such patients sustain cystitis and there appears to be no other effective therapies. The cystitis is viral in etiology (polyoma virus). I attach 3 abstracts of small series of cases treated with HBO2. with a good reported response. I note that they typically report response after about 10 treatments. I did not see that patients have received more than 40 treatments.
- Hemorrhagic cystitis due to polyomavirus abstracts
- Clinical effectiveness of hyperbaric oxygen therapy for BK-virus-associated hemorrhagic cystitis after allogeneic bone marrow transplantation
J Savva-Bordalo1, C Pinho Vaz1, M Sousa1, R Branca1, F Campilho1, R Resende2, I Baldaque3, O Camacho2 and A Campos1
Bone Marrow Transplantation (2012) 47, 1095 -- 1098 & 2012 Macmillan Publishers Limited All rights reserved 0268-3369/12
www.nature.com/bmt
We have a patient who was initially treated with external beam radiation for prostate cancer. About 5 years later he was found to have a recurrence of this cancer and was treated with Radioactive Beads. He now has issues Radiation Cystitis associated with pain and hematuria. However he was found on the last cystoscopy/TURP to have areas of necrotic tumor on his prostate. The Urologist has referred him for HBO therapy for the symptomatic Radiation Cystitis. Are there contraindications for HBO ther
Posted: 12/7/2010
Q:
We have a patient who was initially treated with external beam radiation for prostate cancer. About 5 years later he was found to have a recurrence of this cancer and was treated with Radioactive Beads. He now has issues Radiation Cystitis associated with pain and hematuria. However he was found on the last cystoscopy/TURP to have areas of necrotic tumor on his prostate. The Urologist has referred him for HBO therapy for the symptomatic Radiation Cystitis. Are there contraindications for HBO therapy for the Radiation Cystitis, while he apparently may have ongoing active Prostate Cancer.
A:
One of the topics that has come up in our center is the concern surrounding treating active cancer (CA) patients. I would really appreciate your thoughts on this topic. From all the studies I've read, there still seems to be a fair amount of ambiguity in this area. Above all, I've yet to read a study where the results are conclusive; whether for or against the usage of HBO2 for the treatment of CA. As a medical director, how do you approach these patients during the initial consultation with regards to the medical legal aspect?
I am attaching the paper I did a number of yrs ago which was fairly comprehensive at that time. Since then there have been a smattering of papers, mostly case reports or pre-clinical studies which are a mixed bag. I am still convinced that the evidence supporting a renewal or acceleration of cancer growth is not at all impressive. I advise those who ask me to include a statement like this in their consent..."While the vast majority of published papers show no evidence of cancer recurrence or enhanced growth, based on a few papers with very few patients some authors have expressed their concerns about cancer growth. You should take this information under consideration if you decide to have hyperbaric treatments." Many publications that question the issue of cancer growth and suggest that HBO does enhance growth are directly contradicted by papers of the same or similar design
See attached. It is not a straightforward issue. Some patients with cancer recur and some develop rapid growth (probably after collapse of their inherent immune response.) This happens whether or not they have HBO treatments.”
The paper you attached is https://www.uhms.org/images/MEDFAQs/October-21-2016/Feldmeier_HBO_and_Malignancy.pdf
Also see the additional papers below:
- Hyperbaric Oxygen Therapy for Malignancy: A Review; Jurstine Daruwalla, B.Sc, Chris Christophi, MD; World J Surg (2006) 30: 2112–2131
- Hyperbaric Oxygen: Does it promote growth or recurrence of malignancy?; J. Feldmeier, U. Carl, K. Hartmann, P. Sminia; UHM 2003, Vol. 30, No. 1
- Hyperbaric oxygen therapy and cancer—a review; Ingrid Moen & Linda E. B. Stuhr; Targ Oncol (2012) 7:233–242
We have been treating a pt. with radiation cystitis and his main symptom is extreme pain with urination and also defecation. We are nearing completion of 40 treatment at 2.4 ata x90 minutes. Like oking at our LCD, it says that treatments must be completed in 4-8 weeks. This patient has had absolutely no changes in symptoms. Has anyone achieved results going beyond 40 treatments? Is it even possible to go beyond 40 and have insurance approve it?
Posted: 12/7/2020
Q:
We have been treating a pt. with radiation cystitis and his main symptom is extreme pain with urination and also defecation. We are nearing completion of 40 treatment at 2.4 ata x90 minutes. Like oking at our LCD, it says that treatments must be completed in 4-8 weeks. This patient has had absolutely no changes in symptoms. Has anyone achieved results going beyond 40 treatments? Is it even possible to go beyond 40 and have insurance approve it?
A:
We had two physician experts comment on your questions, Drs. John Feldmeier and Helen Gelly. Both were kind enough to share their knowledge and experiences that we hope you’ll share with your physician team members. Additionally, Dr. Feldmeier has several questions to help us better understand the clinical situation.
My experience has been that radiation cystitis is often refractory or at least slow to respond to HBO2 treatment and commonly requires more than 40 treatments. I know of several cases treated to 60 plus and even 90 treatments before signs and symptoms resolved. I have also seen several cases where patient have recurred with hematuria in a few months post initial treatment and good initial response. These usually will respond to a second course of HBO2
When you say the patient has not improved, have you been tracking any objective signs? If the patient had had any anemia, is this improving? If the patient had required transfusion previously, has this improved? Has the hematuria improved? Is the patient on anti-coagulants for atrial fibrillation or following deep venous thrombosis or PE? Has the patient had cystoscopy?
I would review the patient's meds and see if any of them tend to cause abnormal bleeding. If they can be decreased in dose or preferably D/Ced, I would do so after the concurrence of the physician who started the meds. I also recommend that the patient have a cystoscopy at this time. You need this to make sure that there is no malignancy causing the bleeding and also if there is one or just a few troublesome sites a local electrocautery or laser photo coagulation might be in order. At any rate having a direct visualization and comparison if cystoscopy was done prior to HBO2 will give valuable information as to whether there has been an improvement. This information may also help in making a case to the insurer for more HBO2 if some improvement is seen.. Again, in my experience, often cystitis requires more than 40 treatments, but if there truly has been no response other causes or complicating factors need to be considered.
The first thing is that I would have the urologist do another cystoscopy. With bladders and bowel you are truly blind as to progress, and unless you are following them closely you can miss a local recurrence or a new primary. Also, from a payment standpoint, if you are going to exceed 60, you better have evidence of improvement, and the only way to do that is to scope them.
I would be concerned that there is not a greater impact at 40.
From a payment perspective, after 60, they need to be prepared to defend any more treatments, and that will require independent evidence.
And I agree that you have to rule other causes of persistent bleeding and pain ( all of John's suggestions are excellent), we had one guy that got better through the week and then would come back worse after the weekend and we finally figured out that he would not hydrate (to decrease urination) and then ride his lawnmower for hours over rough terrain. But that is anecdotal.
Is vitamin E is a reasonable approach to preventing oxygen toxicity seizures in a patient on chronic prednisone?
Posted: 9/3/2020
Q:
Is vitamin E is a reasonable approach to preventing oxygen toxicity seizures in a patient on chronic prednisone?
A:
There is no current evidence that Vitamin E is an appropriate prophylactic in mitigating CNS oxygen toxicity during HBO2, and there is also no reported evidence that steroids increase CNS oxygen toxicity risk during HBO2.
My partner and I are working on an HBO safety profile for a patient that may benefit from HBO. The patient is currently treated with cabazitaxel. Please see details below and if you have time, please weigh in as to the safety of this chemo and HBO combination.
Posted: 8/27/2020
Q:
My partner and I are working on an HBO safety profile for a patient that may benefit from HBO. The patient is currently treated with cabazitaxel. Please see details below and if you have time, please weigh in as to the safety of this chemo and HBO combination.
He is a 68 year old seeking HBOT for radiation proctitis and radiation cystitis with hematuria in the setting of chronic anticoagulation (Eliquis) for history of PE. Metastatic disease to lymph nodes currently treated with cabazitaxel every three weeks. Has been tolerating this well (has undergone 11 cycles to date) and associates treatment symptoms with Neulasta.
A:
This particular drug was not used commonly in my experience but it may have become more popular since I have retired. On of its indications is for prostate cancer. Prostate cancers do not respond to chemotherapies well in general and this drug is second line even for that tumor. It interferes with the mitosis of cancer cells by interfering with the disassembly of the microtubules which is necessary for the movement of the chromosomes during mitosis to 2 poles to allow for cellular division. My reference textbook says that 80% of the drug has been eliminated from the body within 2 weeks of an IV infusion. Its main side effects are blood count suppression, mausea and vomiting, fatigue, peripheral nerve toxicity, myalgias and arthralgias, cardiac toxicities, hematuria and dysuria. This drug itself can cause hematuria. I am assuming your patient has had radiation? If so the hematuria is complex with the drug, radiation and anti-coagulants all contributing to the hematuria and making it more likely to be refractory to treatment.
See link below for one abstract where Taxol (the original Taxane) was used in a clinical protocol with HBO. It would appear to me that your patient is not receiving concurrent chemotherapy but has had the drug before.
I don't think that there is a high likeihood of worsened side effects with HBO.John Feldmeier, DO
Systemic chemotherapy using paclitaxel and carboplatin plus regional hyperthermia and hyperbaric oxygen treatment for non-small cell lung cancer with multiple pulmonary metastases: preliminary results
Takayuki Ohguri 1, Hajime Imada, Hiroyuki Narisada, Katsuya Yahara, Tomoaki Morioka, Keita Nakano, Yasuhiro Miyaguni, Yukunori Korogi
For patients with a history of seizure(s), is there literature to define their risk for an O2-induced seizure? Is there any sort of consensus on how to alter a treatment protocol such as increased number of air breaks or treatment depth? Are there thresholds to clear to treat such as length of time to be seizure-free (on or off antiseizure meds)? Or is such a patient at the same risk as any other patient? I realize that each seizure patient may be different (focal vs. generalized and not a question of rem
Posted : 12/7/2020
Q:
For patients with a history of seizure(s), is there literature to define their risk for an O2-induced seizure? Is there any sort of consensus on how to alter a treatment protocol such as increased number of air breaks or treatment depth? Are there thresholds to clear to treat such as length of time to be seizure-free (on or off antiseizure meds)? Or is such a patient at the same risk as any other patient? I realize that each seizure patient may be different (focal vs. generalized and not a question of remote h/o febrile seizure in childhood).
For patients with a history of seizure(s), is there literature to define their risk for an O2-induced seizure?
- Hyperbaric Oxygen Therapy: Side Effects Defined and Quantified; Marvin Heyboer III,* Deepali Sharma,William Santiago, and Norman McCulloch; ADVANCES IN WOUND CARE, VOLUME 6, NUMBER 6
- Seizure incidence by treatment pressure in patients undergoing hyperbaric oxygen treatment; Marvin Heyboer III, Shane Jennings, William D. Grant, Cindy Ojevwe, Joseph Byrne, Susan M. Wojcik; UHM 2014, Vol. 41, No. 5
- Oxygen toxicity seizures: 20 years' experience from a single hyperbaric unit; Neil D G Branham; Diving and Hyperbaric Medicine, Vol 41, No. 4, December 2011
Is there any sort of consensus on how to alter a treatment protocol such as increased number of air breaks or treatment depth?
A: No. Practically speaking one may decreased depth, decrease length, and add air breaks. No study has demonstrated efficacy, but it makes theoretical sense.
Are there thresholds to clear to treat such as length of time to be seizure-free (on or off antiseizure meds)?
A: No. Recommendation is stable on anti-seizure medication. Epilepsy has never been identified as an actual risk factor although theoretical risk.
Or is such a patient at the same risk as any other patient?
A: Literature says same risk, but not unreasonable during informed consent to acknowledge possible increased risk.
There is no formula for adjusting a dive profile to decrease the likelihood of having a seizure. Likewise, there is no model, formula or nomogram that forecasts the likelihood of an oxygen induced seizure when patient presents with a history of seizure disorder. The important thing is to make sure that the patient’s seizure medications are appropriately dosed and taken by the patient. Blood levels if available should be obtained. We assume that O2 induced seizures are more likely when patients with an underlying seizure disorder (or fever) is present but even that assumption is mostly an educated guess.
In terms of adjusting the profile, of course it depends on the pressure you are using for treatment and what the disorder being treated is. If it is a 2.4 ATA profile I would begin increasing the frequency of air breaks to every 20 minutes for a 5 minute duration. If a seizure occurs there, I would reduce the pressure to 2.0 ATA and continue air breaks (probably every 30 minutes). I would avoid any futher reduction of pressure if possible.
If it is a 2.0 ATA profile I would introduce air breaks if none are being used. I would begin with 5 minutes every 30 minutes. If a seizure occurs I would introduce the air breaks every 20 minutes for 5 minutes. I would not reduce pressure downward from 2.0 ATA.
If it is a 2.8 or 3.0 ATA profile, I would increase the frequency of air breaks, but a stepwise pressure decrease might be needed as well. Obviously, these treatments would be for a diving case or perhaps a gas gangrene or necrotizing fasciitis. In that case pressures should be maintained if at all possible and the best option is to increase the frequency of air breaks. Care should be taken in ascending to a lower pressure especially in a table VI or other similar profile for DCS so as to not make the DCS or Air Embolism worse.
I hope this provides you with some guidance. In my experience, it is an empirical adjustment. Obviously, you will have selected a particular treatment profile because you thought it was appropriate for that patient. I would avoid radical changes and make only minor adjustments. In my experience, the shortening of O2 periods and increased frequencies of air breaks usually works well.
How long do the effects of HBO for osteoradionecrosis last? E.g. a patient was treated for ORN (40 sessions) four years ago, needs repeat oral surgery, would warrant re-treatment with Marx protocol 20+10? What about if it was only 2 years ago?
Posted: 7/31/2020
Q:
Title: How long do the effects of HBO for osteoradionecrosis last? E.g. a patient was treated for ORN (40 sessions) four years ago, needs repeat oral surgery, would warrant re-treatment with Marx protocol 20+10? What about if it was only 2 years ago?
A:
Bob Marx is of the opinion that once a patient completes a full course of HBO2 he or she does not need to repeat again EXCEPT if there is actual radionecrosis. If it is to support a dental extraction or implant, there would be no need for more HBO2. Bob Johnson who has been Bob Marx's collaborator on much of their joint efforts would say that if at the time of the oral surgery the tissues did not appear well-vascularized, it would be appropriate to give 10 post procedure treatments but with out the pre-op sessions. BUT, if there is bony necrosis present a second full 30 and 10 would be the best course.
I am currently treating a patient with breast cancer for a lower extremity wound due to late effects of radiation. Ibrance has been held due to known effects on wound healing. She has completed #20 HBOT. Wound has shown some improvement, but not yet resolved. Patient's oncologist would like to resume Ibrance. Are there any relative or absolute contraindications to continuing HBOT once Ibrance is resumed?
Posted: 7/14/2020
Q:
I am currently treating a patient with breast cancer for a lower extremity wound due to late effects of radiation. Ibrance has been held due to known effects on wound healing. She has completed #20 HBOT. Wound has shown some improvement, but not yet resolved. Patient's oncologist would like to resume Ibrance. Are there any relative or absolute contraindications to continuing HBOT once Ibrance is resumed?
A:
Please see the following paper: Ibrance (Palbociclib) and Hyperbaric Oxygen
It does look like this drug might interfere with wound healing although probably no more so than many other chem drugs. There is nothing found on a literature search of the two together.
I would predict no enhancement of toxicity with the caution that without any published experience that prediction is no more than an educated guess based on a review of the drug's characteristics. As I always try to do, I also add the caution that the treating physician must take responsibility for any unexpected enhanced toxicities when HBO2 is given to a patient on this drug.
I would like to start my 57-year-old patient on HBO therapy for soft tissue radiation injury. He completed chemotherapy and radiation for treatment of rectal cancer about 21 months ago. Since that time, he struggled with perianal cutaneous ulcers. I think HBO will help. I want to make sure the FOLFOX and 5-FU chemotherapy he completed 21 months ago does not complicate his case. I do not think they do, I am sure they have cleared his system.
Posted: 7/6/2020
Q:
I would like to start my 57-year-old patient on HBO therapy for soft tissue radiation injury. He completed chemotherapy and radiation for treatment of rectal cancer about 21 months ago. Since that time, he struggled with perianal cutaneous ulcers. I think HBO will help. I want to make sure the FOLFOX and 5-FU chemotherapy he completed 21 months ago does not complicate his case. I do not think they do, I am sure they have cleared his system.
A:
None of the drugs in the FOLFOX multi-drug protocol given nearly 2 years ago should complicate your intent to give HBO2
for perianal ulcers, presumably caused by radiation.
Please, remember that the cancer itself can cause fistulas to the skin of the perineum. Just cautioning that you make sure that he has no active cancer because the cancerous wounds will not heal using HBO2.
A patient that is likely going to start HBO2 soon, presented a model number of his intraocular lens implant (MI60L). While I think this is okay, I would like to check since he has the model number from Bausch & Lomb. How can I determine if this posterior chamber implant is compatible with HBO2 Therapy?
Posted: 7/1/2020
Q:
A patient that is likely going to start HBO2 soon, presented a model number of his intraocular lens implant (MI60L). While I think this is okay, I would like to check since he has the model number from Bausch & Lomb. How can I determine if this posterior chamber implant is compatible with HBO2 Therapy?
A:
Most of the issues of eye surgery and immersed diving are largely irrelevant in the dry hyperbaric environment unless there are intraocular gas bubbles as mentioned below.
Air bubbles are sometimes present in the eye for a few days after cataract surgery and their absence should be specifically documented by the ophthalmologist prior to HBO2 if the HBO2 takes place shortly after cataract surgery.
There is no physiological reason that I am aware of that would mandate a waiting period for an HBO2 treatment after cataract surgery in the absence of an intraocular gas bubble.
I am unaware of any reports of negative effects of HBO2 on intraocular lens implants. I have also never heard of patients who have intraocular lens implants experiencing a myopic shift as a result of HBO2 treatments, as many patients with their natural lens still in place do.
As always, I would suggest that the patient discuss this information with the ophthalmologist responsible for their care.
I have a patient that I am trying to get approved for HBO. His radiation dose was 5040 over 28 treatments to his pelvis for colorectal CA. Is he a good candidate based on his dose? It seems that it may be a bit low (thinking 6000 cut off).
Posted: 6/24/2020
Q: I have a patient that I am trying to get approved for HBO2. His radiation dose was 5040 over 28 treatments to his pelvis for colorectal CA and is having continuous perianal skin breakdown for one year. Is he a good candidate based on his dose? It seems that it may be a bit low (thinking 6000 cut off).
A: The perineal area when included in the treatment volume is a tough area to heal. I think the dose is adequate to cause these problems and the material fact is that there are non-healing tissues and that they are persistent at a year.
In a person with heavy alcohol dependence, is there a concern of alcohol withdrawal seizures during HBO therapy for a different condition (i.e. STRN, etc)? If so, has this risk been described or quantified, and would expert consensus recommend using a specific chamber class (multiplace vs monoplace) to treat an approved indication, given this comorbidity? Thank you.
Posted: 8/11/2020
Q:
In a person with heavy alcohol dependence, is there a concern of alcohol withdrawal seizures during HBO therapy for a different condition (i.e. STRN, etc)? If so, has this risk been described or quantified, and would expert consensus recommend using a specific chamber class (multiplace vs monoplace) to treat an approved indication, given this comorbidity?A:
A:
In regard to dealing with alcohol withdrawal and hyperbaric treatment for non-emergent indications, it seems to me that the most prudent course of action is to delay treatment until the patient has gone through the process of withdrawal with all its attendant physiologic and neuropsychiatric problems. I personally would not want to deal with a patient in the chamber in this state. After the process of withdrawal has been completed the patient should be fine for treatment. Just as in other patients, if he or she is agitated or claustrophobic, a benzodiazepine anxiolytic would be in order.
Many alcoholic patients have been treated with HBO2 over the years. Although alcohol abuse may theoretically reduce threshold for seizure activity, it has not been a common problem.
Below is an abstract that suggests based on very limited anecdotal experience that alcohol withdrawal may lower the threshold for O2 induced seizure.
Risk Factors for Oxygen Toxicity Seizures in Hyperbaric Oxygen Therapy: Case Reports From Multiple Institutions
Ruthanna Seidel 1, Christopher Carroll 2, Debra Thompson 2, Rena G Diem 2, Kwabena Yeboah 2, A J Hayes 2, Brett Hall 2, Harry T Whelan 2
Affiliations
· 1University of Arizona College of Medicine, Phoenix, Phoenix, Arizona, USA.
· 2Medical College of Wisconsin, Milwaukee, Wisconsin, USA.
· PMID: 24377194
Abstract
Oxygen toxicity seizures are a rare but recognized complication of hyperbaric oxygen (HBO2) therapy. Many patients undergoing HBO2 therapy have medical conditions or are taking medications that could contribute to seizures. Previous literature has not extensively reported on these factors in patients experiencing oxygen toxicity seizures. We conducted a chart review at several hyperbaric oxygen centers in the Milwaukee, Wisc., area to explore whether the patients who experienced seizures in the hyperbaric chamber had other medical comorbidities or were on medications which lowered their seizure threshold, thereby contributing to oxygen toxicity seizures. There were a total of seven cases of seizures in five patients. Each patient had risk factors for seizures, including hypercapnia secondary to chronic obstructive pulmonary disease, narcotic withdrawal, alcohol dependence, and antidepressant, tramadol or cephalosporin/ceftriaxone use. We hypothesize that patients who experience oxygen toxicity seizures may have other factors which contribute to the development of these seizures.
i have a pt that we are working up for HBO. He has a significant psych history, including schizophrenia. He is taking quetiapine citalopram, and trazodone. Will these medications have a safe interaction with the high concentration of oxygen?
Posted: 12/7/2020
Q:
I have a pt that we are working up for HBO. He has a significant psych history, including schizophrenia. He is taking quetiapine citalopram, and trazodone. Will these medications have a safe interaction with the high concentration of oxygen?
A:
There are no specific published experiences of these three agents. In the latest version of the Kindwall textbook, Hyperbaric Medicine Practice. Dr. Ryan Feldman in his article in the Kindwall textbook (page 149, 4th Edition) discusses the issue of psychotopics and HBO2. One mechanism for their effects is the increase of serotonin levels in the CNS in the synaptic space by interfering with cellular reuptake. The chapter in the Kindwall textbook discusses chloropromazine and prochlorpromazine specifically and notes that have been reported to reduce oxygen toxicity.
In regard to the drugs you are inquiring about, I have the following remarks:
Quietapine (Seraquel)also works through serotonin receptors. Quietapine’s side effects include low blood pressure with standing, seizures, a prolonged erection, high blood sugar, tardive dyskinesia, and neuroleptic malignant syndrome.
Theoretically, a patient receiving HBO2 and this drug might have a lower threshold for seizure onset. Consideration should be given to alteration in the HBO2 treatment profile to decrease the likelihood of seizures.
Citalopram (Celexa): It is an SSIR (Selective Serotonin Reuptake Inhibitors)like Quietadine.
Listed below are conditions that patients are advised to discuss with their physicians before starting Citalopram.
- a bleeding or blood clotting disorder;
- liver or kidney disease;
- narrow-angle glaucoma;
- seizures or epilepsy;
- heart disease, heart failure, a heart rhythm disorder, slow heartbeats, or recent history of heart attack;
- personal or family history of Long QT syndrome;
- an electrolyte imbalance (such as low levels of potassium or magnesium in your blood);
- bipolar disorder (manic depression); or
- a history of drug abuse or suicidal thoughts.
To me the list implies a likely increase of risk for seizure as above for Quietapine. As above the patient should be carefully observed for any prodromes of a seizure while in the chamber and consideration could be given to altering the HBO2 protocol to reduce the risk of seizure.
Trazadone
At higher dose Trazadone also can act as an SSIR.
Its list of more common cautions for Trazadone include:
- Bipolar disorder
- Kidney or liver disease
- Blood or bleeding disorders
- Heart disease
- A heart rhythm problem called long QT syndrome
- Low blood pressure
- Low blood sodium
- Recent heart attack
No indication that I could find indicated that it too presented a risk for seizures.
In terms of how to put this all together, we can only say that psychotropics have been used with HBO2 before without significant complications. Trazadone and Celexa are common drugs and I have to believe that they have been given with HBO2 before and nor reports of negative interaction of these drugs was found on literature search.
Two of the 3 drugs seem to have a risk for seizure. I would probably begin the patient at 2.0 ATA and introduce airbreaks every 30 minutes. If he or she does well, you might then consider increasing pressure or length of O2 treatment.
As always, the decision to treat or not treat is the purview of the hyperbaric physician and our remarks are only meant to provide what information is discoverable.
I have a patient with severe Crohn's disease and multiple abdominal wall fistulas that has been told she is not a surgical candidate. She is already on TPN with limited liquid PO. Does anyone have advice for treatment protocols, length of course, things to look out for, etc.?
Posted: 12/7/2020
Q:
I have a patient with severe Crohn's disease and multiple abdominal wall fistulas that has been told she is not a surgical candidate. She is already on TPN with limited liquid PO. Does anyone have advice for treatment protocols, length of course, things to look out for, etc.?
A:
There are numerous small case series reporting the results of hyperbaric oxygen in the treatment of inflammatory bowel disease (Crohns and Ulcerative Colitis). Typically these are positive in results for a majority of cases often including patients refractory to pharmacologic treatment and in Crohns including patients with fistulae.
Below is a review article that summarizes much of the literature and gives details on treatment protocols used. Toxicities have been very rare and generally the typical side effects encountered in the clinical practice of hyperbaric oxygen.
Hyperbaric oxygen treatment for inflammatory bowel disease: a systematic review and analysis; Daniel A Rossignol; Rossignol Medical Gas Research 2012, 2:6
I have a question for management of CRAO patients who are hospitalized for HBOT: This presupposes the patient showed some response to the first dive. Due to staffing limitations, we treat CRAO patients who respond to first treatment (but have not returned to normal vision) on a BID basis until plateau has been reached. I am interested in best evidence to support use of supplemental normobaric oxygen between HBOT. I would be interested in other facilities approach. A related question is how other facilitie
Posted: 12/15/2020
Q:
I have a question for management of CRAO patients who are hospitalized for HBOT: This presupposes the patient showed some response to the first dive. Due to staffing limitations, we treat CRAO patients who respond to first treatment (but have not returned to normal vision) on a BID basis until plateau has been reached. I am interested in best evidence to support use of supplemental normobaric oxygen between HBOT. I would be interested in other facilities approach.
A:
For patient's being treated for CRAO (Central Retinal Artery Occlusion) with BID HBO2, what is the best evidence for dosing and frequency of normobaric supplemental oxygen between HBOT treatments?
This answer is from Dr. Heather Murphy-Lavoie who has published and spoken extensively on this topic:
“The patient should be treated BID at the of return of vision or 2.8ATA if no improvement. Treat until no further improvement for three days or recanalization proven by fluorescein angiogram. Between treatments patients should ideally be admitted to the hospital on a stroke protocol where they can be monitored. Oxygen is given for 15 min every hour only if it is needed to maintain viability of the retina between treatments. The Hyperbaric Oxygen Therapy Indications Manual, 14th Edition has more detail on this subject.”
A recent article, “Tauchen nach Covid-19-Erkrankung?” concludes that divers who have had COVID-19 will be permanently unfit to dive. Is this opinion shared by diving medical professionals? What is the evidence?
Posted: 4/24/2020
QUESTION:
A recent article, “Tauchen nach Covid-19-Erkrankung?” concludes that divers who have had COVID-19 will be permanently unfit to dive. Is this opinion shared by diving medical professionals? What is the evidence?
ANSWER:
At the present time, we simply do not have sufficient data to support or refute the definitive proclamations made by this case series. Any attempt to generalize the effects of COVID-19 based upon a single case series (6-cases) published in the lay-press1,2, should be met with appropriate scrutiny.
Covid-19 symptoms range from mild to severe. Some people have no symptoms at all while others require complicated stays in an intensive care setting and require ventilatory support. The recent report published in the lay-press1,2 has resulted in considerable concern related to the finding of pulmonary inflammation in mild cases of COVID-19. This case series reports findings that may provide some insight into post-infection recovery, with a potential knock-on effect on fitness to dive evaluations, and recommendations related to medical follow up studies, and convalescence period prior to a return to diving. However, we must interpret this small case series (6-cases) with caution, as there is not enough known about the natural history of this disease to confidently extrapolate prognostic guidance from this one report, nor generalize these findings to every case of COVID-19. Likewise, calls for a particular medical examination or screening test(s) following infection to determine fitness to dive, based on this work alone, are currently unsubstantiated and premature.
The list of potential variables related to how this disease manifests, its clinical course, and longterm prognosis is lengthy and may include factors such as underlying medical conditions, age, disease severity, and secondary complications. Case reports suffer from multiple design weaknesses to include a lack of controls and randomization, which makes any conclusions that we may want to generalize to a larger population suspect. While these findings are indeed disquieting, it will take time before the potential impact on individual health, and any lasting effects on lung or heart function, are captured in the peer-reviewed literature.
COVID-19 shares many of the same features as other serious viral pneumonias that require a period of convalesce before returning to full activities – a process that can take weeks or months depending on symptom severity. The long-term effects of COVID-19 on pulmonary function and recovery time will vary, and there is insufficient experience and sound clinical research to make accurate prognostic determinations.
As the diving medical community gains more experience, and has the opportunity to study this illness and follow patients through their recovery, we will develop a thoughtful approach to making fitness to dive determinations. A single small case series is insufficiently powered to support definitive statements related to permanent lung function changes or air trapping risk – but these are unquestionably areas of keen interest within the diving medical community and will be closely monitored.
Over the next several months, the global medical community will gain a better understanding of the natural history of this disease. In addition, multiple studies are underway looking at treatment modalities and how we may reduce morbidity and mortality. COVID-19 has gripped the world and there is no other time in our history where we have as many people searching for answers about a single disease. We will continue to track research on this topic and update this position as new information becomes available.
_________________________________
- Hartig, Frank. Tauchen nach Covid-19-Erkrankung? Wetnotes. April 15, 2020. https://www.wetnotes.eu/tauchen-nach-covid-19-erkrankung/
- (Translation of reference 1). Bandera County Courier. Medic sees evidence of serious long-term lung damage. April 18, 2020. https://www.bccourier.com/medic-sees-evidence-of-serious-long-term-lung-damage/
- Hughes, Russel. COVID-19 potential impact on divers. Advanced Diving NZ. April 21, 2020.https://www.advanceddivingnz.com/advanced-diving-blog/2020/4/21/covid-19-potential-impact-on-divers?fbclid=IwAR2bhP-kXvUYCKNQu8a-tpzlMQf6YKX2m1AlPlYYZadEYrWGZKu0sroTCEk.
I had COVID-19. Will I be able to return to diving?
Posted: 4/23/2020
QUESTION:
I had COVID-19. Will I be able to return to diving?
ANSWER:
At the present time, we simply do not have sufficient data to support or refute the definitive proclamations made by this case series. Any attempt to generalize the effects of COVID-19 based upon a single case series (6-cases) published in the lay-press1,2, should be met with appropriate scrutiny.
Covid-19 symptoms range from mild to severe. Some people have no symptoms at all while others require complicated stays in an intensive care setting and require ventilatory support. The recent report published in the lay-press1,2 has resulted in considerable concern related to the finding of pulmonary inflammation in mild cases of COVID-19. This case series reports findings that may provide some insight into post-infection recovery, with a potential knock-on effect on fitness to dive evaluations, and recommendations related to medical follow up studies, and convalescence period prior to a return to diving. However, we must interpret this small case series (6-cases) with caution, as there is not enough known about the natural history of this disease to confidently extrapolate prognostic guidance from this one report, nor generalize these findings to every case of COVID-19. Likewise, calls for a particular medical examination or screening test(s) following infection to determine fitness to dive, based on this work alone, are currently unsubstantiated and premature.
The list of potential variables related to how this disease manifests, its clinical course, and longterm prognosis is lengthy and may include factors such as underlying medical conditions, age, disease severity, and secondary complications. Case reports suffer from multiple design weaknesses to include a lack of controls and randomization, which makes any conclusions that we may want to generalize to a larger population suspect. While these findings are indeed disquieting, it will take time before the potential impact on individual health, and any lasting effects on lung or heart function, are captured in the peer-reviewed literature.
COVID-19 shares many of the same features as other serious viral pneumonias that require a period of convalesce before returning to full activities – a process that can take weeks or months depending on symptom severity. The long-term effects of COVID-19 on pulmonary function and recovery time will vary, and there is insufficient experience and sound clinical research to make accurate prognostic determinations.
As the diving medical community gains more experience, and has the opportunity to study this illness and follow patients through their recovery, we will develop a thoughtful approach to making fitness to dive determinations. A single small case series is insufficiently powered to support definitive statements related to permanent lung function changes or air trapping risk – but these are unquestionably areas of keen interest within the diving medical community and will be closely monitored.
Over the next several months, the global medical community will gain a better understanding of the natural history of this disease. In addition, multiple studies are underway looking at treatment modalities and how we may reduce morbidity and mortality. COVID-19 has gripped the world and there is no other time in our history where we have as many people searching for answers about a single disease. We will continue to track research on this topic and update this position as new information becomes available.
_________________________________
- Hartig, Frank. Tauchen nach Covid-19-Erkrankung? Wetnotes. April 15, 2020. https://www.wetnotes.eu/tauchen-nach-covid-19-erkrankung/
- (Translation of reference 1). Bandera County Courier. Medic sees evidence of serious long-term lung damage. April 18, 2020. https://www.bccourier.com/medic-sees-evidence-of-serious-long-term-lung-damage/
- Hughes, Russel. COVID-19 potential impact on divers. Advanced Diving NZ. April 21, 2020. https://www.advanceddivingnz.com/advanced-diving-blog/2020/4/21/covid-19-potential-impact-on-divers?fbclid=IwAR2bhP-kXvUYCKNQu8a-tpzlMQf6YKX2m1AlPlYYZadEYrWGZKu0sroTCEk.
What are the current guidlines for a non insulin dependent patient in a monoplace chamber?
Posted: 4/22/2020
We do not have guidelines for the management of diabetics in the chamber however there are a number of resources available to you, including the attached BNA Nursing Guidelines, Best Publishing’s Policy and Procedural Guidelines for Hyperbaric Facilities (2022) published a recommended scale in policy #304 on page 51 and Best Publishing Company’s Hyperbaric Medicine Practice, 4th Edition (2017) on page 126 in the Hyperbaric Nursing chapter and on page 144 in The Use of Drugs Under Pressure chapter, the topic is covered.
HBOT for COVID Cytokine storm: Is there any reasonably valuable anecdotal evidence of HBOT benefit for COVID-19 or Sars-1?
Posted 4/3/2020
Q:
HBOT for COVID Cytokine storm: Is there any reasonably valuable anecdotal evidence of HBOT benefit for COVID-19 or Sars-1?
A:
The UHMS website has an extensive section addressing the issue of HBO2 for COVID-19. The portion of this posting that deals with the rationale for treatment including mechanisms extensively deals with the questions asked above. We do indeed believe that HBO2 can have a favorable impact on the cytokine storm and especially through its anti-inflammatory effects reduce the exaggerated immune response that is at the heart of damage caused by the infection. Please refer to this posting.
HBOT for COVID Cytokine storm 1 )It is reported patients suffering from COVID-19 have elevated levels of many cytokines (IL-1,2,4,7,10,12,13,17, GCSF, TNF, others). Could HBOT not down regulate this response to mitigate the resultant ARDS? If so, should HBOT be implemented in patients not yet intubated but at risk, and how do we identify? Or should it be used for those with ARDS on vent support, and when to initiate, early or late? 2) Aside from the cytokine storm question, what of the role of HBOT in
Posted 4/3/2010
Q: HBOT for COVID Cytokine storm
1 )It is reported patients suffering from COVID-19 have elevated levels of many cytokines (IL-1,2,4,7,10,12,13,17, GCSF, TNF, others). Could HBOT not down regulate this response to mitigate the resultant ARDS?
If so, should HBOT be implemented in patients not yet intubated but at risk, and how do we identify?
Or should it be used for those with ARDS on vent support, and when to initiate, early or late?
2) Aside from the cytokine storm question, what of the role of HBOT in the supportive role of mitigating hypoxic end organ injury?
A:
The UHMS website has an extensive section addressing the issue of HBO2 for COVID-19. The portion of this posting that deals with the rationale for treatment including mechanisms extensively deals with the questions asked above. We do indeed believe that HBO2 can have a favorable impact on the cytokine storm and especially through its anti-inflammatory effects reduce the exaggerated immune response that is at the heart of damage caused by the infection. Please refer to this posting.
Has there been any research to see if there are contraindications to a female patient being dove to 2.4 ATA with a Mirena IUD in place? Will the change in ATA cause an increase or decrease in hormone delivery? (Currently 20mg/24 hrs over 5 years) and 2nd, will the change in ATA increase the risk that the IUD will migrate to perferate the uterus?
Date Posted: 3/11/2020
MEDFAQ Question: Has there been any research to see if there are contraindications to a female patient being dove to 2.4 ATA with a Mirena IUD in place? Will the change in ATA cause an increase or decrease in hormone delivery? (Currently 20mg/24 hrs over 5 years) and 2nd, will the change in ATA increase the risk that the IUD will migrate to perferate the uterus?
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
Generally speaking, intrauterine devices are an effective and popular form of birth control. Based upon the frequency of their use, hyperbaric professionals should be prepared to field questions related to the safety of these devices within the unique environment of the hyperbaric chamber.
For the sake of clarity, there are two types of IUDs:
Non-hormonal IUD: These devices are made of copper and may last up to twelve years.
Hormonal IUD: These devices are designed to release small amounts of hormone (typically levonorgestrel) locally into the uterus. Levonorgestrel causes thickening of the cervical mucus and thins the lining of uterus.
In particular, the Mirena IUD is a hormonal IUD that is made of soft, flexible plastic and does not appear to contain gas spaces that could be affected by changes in atmospheric pressure. As such, the rate of hormone release would theoretically remain unchanged. Furthermore, increased atmospheric pressure at standard hyperbaric oxygen therapy pressures between 2.0 and 3.0 ATA is not expected to increase the risk of uterine wall perforation. Unfortunately, there are no confirmed studies, reports or testing of this product by the manufacturer under hyperbaric conditions that would validate these suppositions.
The UHMS Hyperbaric Oxygen Safety Committee therefore suggests that a risk assessment be conducted by the Safety Director and Medical Director of the Hyperbaric Facility for your particular patient. There are several related references that may assist you in completing the risk assessment and determining the proper course of action. Of note, the Divers Alert Network has responded to several inquiries related to these devices from a commercial or scuba diving perspective. Their position pertaining to intrauterine devices and diving is that an increase in absolute barometric pressure should have no mechanical effect on the IUD, and there is probably no reason to suspect their hormonal bioavailability or metabolism should be affected. The proportion of female divers diving with a IUD should be no different than that of general population, and DAN has never been made aware of any issues with IUD devices, medicated or not.
Related Articles:
http://www.alertdiver.com/womens_health_and_diving
https://www.diversalertnetwork.org/medical/articles/DAN_Explores_Fitness_and_Diving_Issues_for_Women
http://midlandsdivingchamber.co.uk/index.php?id=advice&page=6&cat=10&sub_cat=11
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
