Greetings from all of us here at UHMS!
As we embark on a new year, I want to thank each of you for your dedication to the field of undersea and hyperbaric medicine. Our work is critical to advancing patient care, improving clinical outcomes, and ensuring the highest safety standards in hyperbaric facilities worldwide. In this first-quarter update, I would like to highlight several key areas that reinforce our commitment to excellence: certification, facility accreditation, hyperbaric system safety, and the value of being a UHMS member.
The Importance of Certification
Certification is a hallmark of professional experience, competency, and commitment to best practices. Whether you are a physician, nurse, or technician, obtaining and maintaining your certification in hyperbaric medicine demonstrates your expertise and adherence to the highest standards of patient care. UHMS strongly encourages physicians in our field to pursue certification through ABPM/ABEM subspecialty board certification or PATH CAQ and NPPs to achieve PATH CAE; we also promote all nurses who participate in the care hyperbaric patients to become Certified Hyperbaric Registered Nurses (CHRN) program, and technicians to be certified as Certified Hyperbaric Technologists (CHT) or Certified Hyperbaric Specialists (CHS). These credentials not only enhance your professional standing but also elevate the credibility of our specialty within the broader medical community.
Please review our position statement on Certification Matters: UHMS POSITION STATEMENT.
Facility Accreditation: A Commitment to Excellence
In light of the recent tragedy in Troy, Michigan, where a 5-year-old little boy died in a horrific chamber fire while his mother stood by helplessly and watched, I will continue to pound the drum that Hyperbaric Facility Accreditation must become mandatory across the board.
Hyperbaric Facility Accreditation by UHMS remains the gold standard for ensuring safety, quality, and adherence to clinical best practices. Accredited facilities demonstrate their commitment to patient safety, operational excellence, and compliance with industry guidelines. If your facility is not yet accredited, I strongly encourage you to explore the process. Not only does accreditation improve patient trust and regulatory compliance, but it also serves as a proactive approach to risk management and liability reduction.
Maintaining Safety Diligence in Hyperbaric Systems
Safety is the foundation of everything we do in hyperbaric medicine. The risks associated with hyperbaric oxygen therapy (HBO2) demand unwavering diligence in maintaining equipment, conducting regular safety drills, and ensuring proper staff training. UHMS provides comprehensive guidelines and resources to help facilities uphold the highest safety standards, including routine inspections, emergency preparedness protocols, and compliance with NFPA 99 and ASME PVHO-1 standards. I urge all members to prioritize safety in daily operations and take advantage of UHMS educational offerings on hyperbaric safety.
The Value of UHMS Membership
Your membership in UHMS is more than just an affiliation—it is an investment in your professional growth and the advancement of hyperbaric medicine. As a UHMS member, you gain access to cutting-edge research, clinical practice guidelines, educational opportunities, networking events, and advocacy efforts to shape our specialty's future. Additionally, membership provides exclusive discounts on conferences, workshops, and certification programs that support your career development.
The UHMS tent is wide open, so please come in and join us to make our specialty vibrant and viable for generations to come!
UHMS Finances
I am pleased to report that UHMS's financial position remains strong.
UHMS experienced a great financial year in 2024, and we ended the year with a robust surplus of $285K, compared to a much smaller surplus in 2023.
| Jan-Dec 2024 PL |
| |
Actual |
Budget |
| Income |
$1,749,850 |
$1,589,607 |
| Expense |
$1,479,906 |
$1,587,568 |
| Net |
$269,944 |
$1,479 |
| Jan 2025 PL |
| |
Actual |
Budget |
| Income |
$156,599 |
$170,601 |
| Expense |
$97,666 |
$106,138 |
| Net |
$58,932 |
$64,462 |
Our balance sheet remains healthy, with operating, savings, and investment accounts continuing to hover at near-all-time highs.
Member Benefits
As a reminder, UHMS members receive three free CE/CME credits upon joining or renewing. This benefit represents an immediate $40 savings for Associate members and $60 for Regular members annually.
Associate Member Town Hall
Members are invited to attend the UHMS Associate Council town hall meeting on the second Thursday of every quarter, where invited speakers present on relevant topics that apply to our specialty.
Corporate Partners
If you are a UHMS Corporate Partner, please attend our monthly Corporate Partner Town Hall meeting series. These are held on the 1st Wednesday of every month at noon and are intended to be an open forum for discussing the challenges and successes your businesses and practices are experiencing and to create momentum and collaboration where appropriate.
If your organization wants to educate the UHMS membership about the care provided or the goods and services offered, consider joining our Corporate Partnership Program. See https://www.uhms.org/corporate-memberships.html.
MEDFAQs
The UHMS offers its version of "ask the experts." MEDFAQs can be found at the following URL – https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq.html, and is a valuable tool for our membership.
If you are familiar with MEDFAQs, check back, as new Q&As are posted regularly.
Research
The UHMS Research Committee continues to be very active. We hope to announce some good news in the new year on the IRB front, where members of our community can come to the UHMS for the Institutional Review Board's needs.
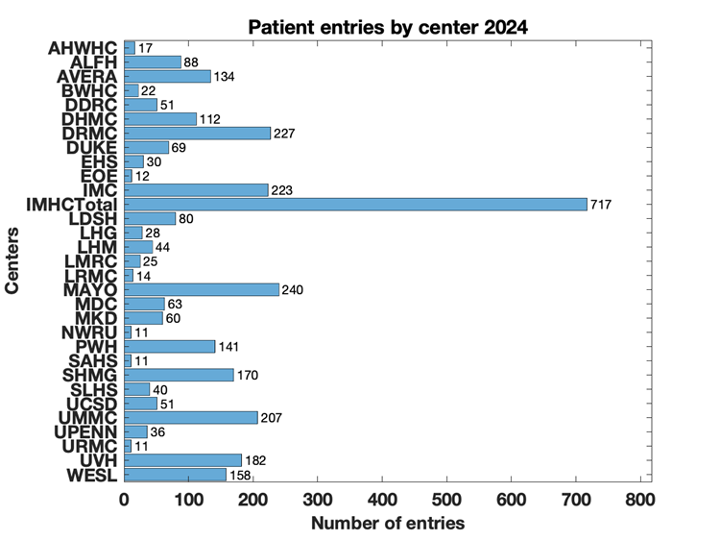
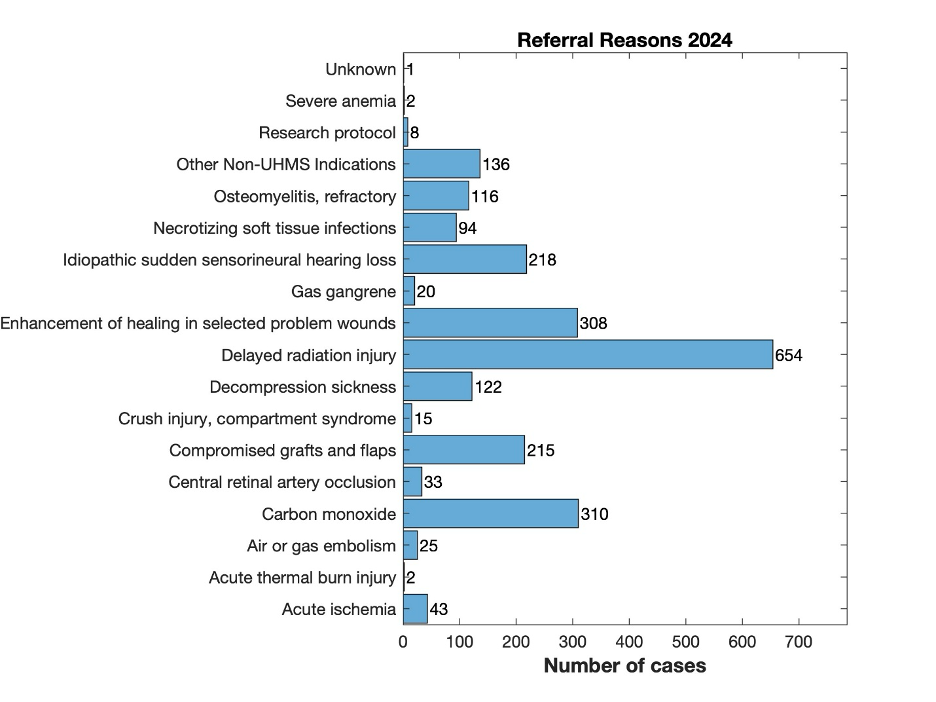
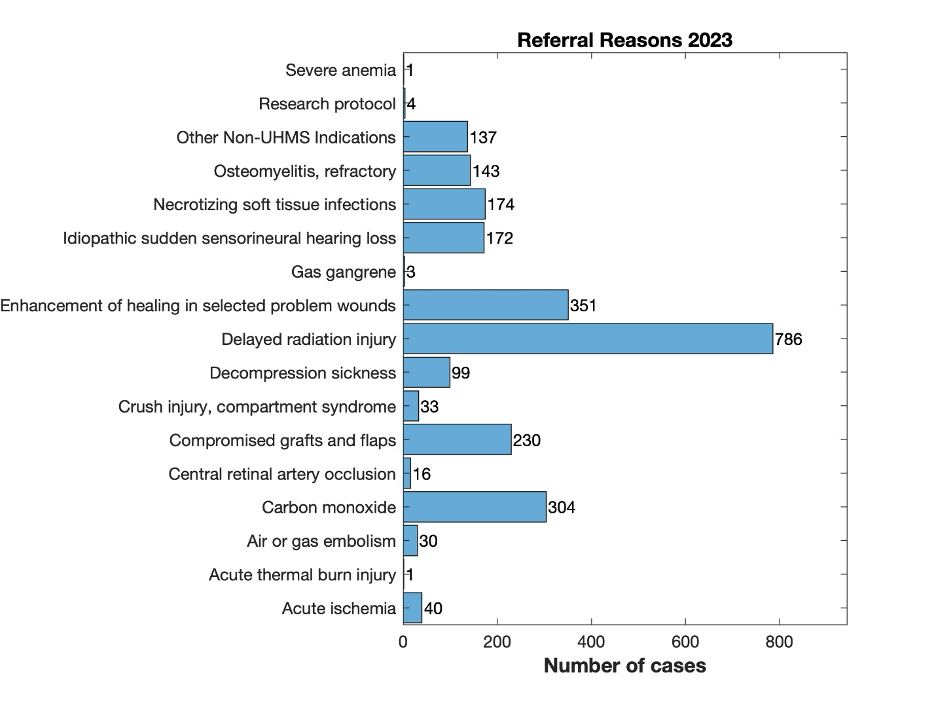
We are soliciting donations from our members for two research initiatives. One is the Continuous Glucose Monitor study (https://www.uhms.org/cgm-hyperbaric-oxygen-study), and the Multicenter Registry for Hyperbaric Oxygen Therapy at Dartmouth (MRHBO2) continues seeking funds for free hospital membership. The MRHBO2 is funded entirely via grants, not by the registry's participating hospitals - https://www.uhms.org/donate-to-the-multicenter-registry-for-hyperbaric-oxygen-therapy.html.
Remember that donations to the UHMS Funds for Research and Policy Advancement are tax-deductible. For more information, check out the UHMS website – https://www.uhms.org/funding.html.
QUARC
To better understand the field's challenges, log in and visit the QUARC page – https://www.uhms.org/resources/quarc.html. Here, you will find impending legislation and other relevant policies on the provision and limitations of HBO2 coverage and the UHMS's responses and guidance.
The chairs of QUARC are requesting that you please let us know as soon as possible if there are any unusual denials or challenges with physicians gaining access to insurance panels for HBO2 services: jpeters@uhms.org.
UHM
If you are a UHMS member, we are happy to announce a new search feature for previous issues and articles from UHM/UBR - https://www.uhms.org/publications/uhm-journal/download-uhm-journal-pdfs.html. Currently, the feature works with keywords.
Looking Ahead
This year, UHMS remains committed to expanding educational initiatives, strengthening industry partnerships, and advocating for policy advancements that benefit our field. We invite you to engage with us, participate in upcoming events, and contribute to the ongoing dialogue that shapes hyperbaric and undersea medicine.
Thank you for being an integral part of our society. Your expertise, dedication, and continued engagement make a difference in advancing the science and practice of hyperbaric medicine.
If you have a suggestion or comment on how we can better serve you, please email me at jpeters@uhms.org or call at 561-776-6110 extension 100.
Sincerely,
John Peters
Executive Director
Undersea and Hyperbaric Medical Society


 Donald Ray Chandler
Donald Ray Chandler